Current Pediatric Research
International Journal of Pediatrics
Study of risk factors and outcome of hypoglycemia in neonates admitted in NICU of a tertiary care hospital in central India.
Dipak Madavi, Manojkumar L Joshi, Milind Suryawanshi, Bhagyashree Tirpude, Lakshmikant Rohadkar*
1Department of Pediatrics, Indira Gandhi Govt. Medical College, Nagpur 440018, India
- Corresponding Author:
- Lakshmikant Rohadkar
Assistant Professor Department of Pediatrics Indira Gandhi Govt. Medical College, Nagpur 440018, India
E-mail: pmbbs13@gmail.com
Received: 13 September, 2023, Manuscript No. AAJCP-23-113555; Editor assigned: 15 September, 2023, Pre QC No. AAJCP-23-113555 (PQ); Reviewed: 06 October, 2023, QC No. AAJCP-23-113555; Revised: 13 October, 2023, Manuscript No. AAJCP-23-113555 (R); Published: 20 October, 2023, DOI:10.35841/0971-9032.27.08.1185-1189.
Background: Neonatal hypoglycemia is a common metabolic disturbance observed during neonatal period. It may be transient asymptomatic event normally occurring as a result of extrauterine adaptation of newborn without any ill effect on somatic or neuronal growth newborn.
Objectives: To determine risk factors and outcome of hypoglycaemia in neonates.
Methods: It was a prospective observational study conducted between December 2020 to November 2022 in the Indira Gandhi Govt. Medical College, Nagpur in Central India. Study population included neonates admitted in Neonatal Intensive Care Unit (NICU) with hypoglycaemia or who had hypoglycaemia during NICU stay. The study was approved by the Institutional Ethical Committee. All the data was entered in excel sheet and results were expressed in terms of number and percentage.
Neonatal Hypoglycemia, Neonatal Intensive Care Unit (NICU), Respiratory Distress Syndrome (RDS), Pregnancy Induced Hypertension (PIH), Prolonged Rupture of Membranes (PROM). 150 neonates with neonatal hypoglycemia satisfying the inclusion and exclusion criteria were enrolled after written informed consent of guardian of the baby. Among 150 hypoglycaemic neonates, number of males 88 (58.67%) was more than females 62 (41.33%). Neonatal risk factors maximum number of babies had septicemia 51 (34%) followed by Respiratory Distress Syndrome (RDS) in 46 (30.67%) babies, Birth asphyxia in 17 (11.33%), meningitis in 11 (7.33%) and twin gestation 9 (6%) in babies with neonatal hypoglycemia. No neonatal risk factor was found in 61 (40.66%) neonates with hypoglycemia. Maternal risk factors Pregnancy Induced Hypertension (PIH) was found in 40 (26.67%) neonates, Prolonged Rupture of Membranes (PROM) in 36 (24%) neonates, Infant of Diabetic Mother (IDM) in 21(14%) neonates, Antepartum Haemorrhage (APH) in 10 (6.67%) neonates. No maternal risk factor was found in 54 (36%) neonates with neonatal hypoglycemia. Majority of discharged babies 123 (93.89%) had normal neurological status and 8 (6.1%) had abnormal neurological status at the time of discharge. Out of 150 hypoglycemic neonates 19 died and mortality was 12.67%.
Conclusion: Present study found prevalence of neonatal hypoglycemia was 17.79%. PIH was found to be the most common maternal risk factor and neonatal septicemia was the most common neonatal risk factor. Most of the babies with hypoglycemia were symptomatic and lethargy was the most common clinical presentation at the time of hypoglycemia. Majority of neonates were discharged with normal neurological status.
Keywords
Neonatal Hypoglycemia, Neonatal Intensive Care Unit (NICU), Respiratory Distress Syndrome (RDS), Pregnancy Induced Hypertension (PIH), Prolonged Rupture of Membranes (PROM).
Abbreviations
RDS: Respiratory Distress Syndrome; PIH: Pregnancy Induced Hypertension; PROM: Prolonged Rupture of Membranes; NICU: Neonatal Intensive Care Unit; APH: Antepartum Haemorrhage; IDM: Infant of Diabetic Mother; GIR: Glucose Infusion Rate;
Introduction
Neonatal hypoglycemia is a common metabolic disturbance observed during neonatal period. It may be transient asymptomatic event normally occurring as a result of extrauterine adaptation of newborn without any ill effect on somatic or neuronal growth newborn [1,2]. Neonatal hypoglycemia may be persistent and symptomatic and have serious effect on somatic and neurodevelopment of newborn [3,4-9]. Neonatal hypoglycemia may be asymptomatic or symptomatic. Symptoms may be subtle and non-specific to hypoglycemia. Most commonly observed symptoms found are poor feeding, jitteriness, lethargy, abnormal respiration, seizures [10]. Infants of Diabetic mother, toxemia of pregnancy, PROM, Antepartum hemorrhage are at increased risk of getting hypoglycemia. LGA babies, SGA babies, IUGR babies, prematurity, neonatal sepsis, birth asphyxia are additional risk factors for neonatal hypoglycemia [11-13]. In a prospective observational study carried out in tertiary care NICU, Prevalence of hypoglycaemia was found to be 14.9% [14]. Persistent and severe hypoglycaemia had serious effects on neurodevelopment of infant. Infants who had hypoglycaemia during neonatal period had increased risk of developmental delay, cerebral palsy, mental retardation in later life [15]. Early detection by screening high risk babies and establishing normoglycemia can prevent deleterious effects of hypoglycaemia on neurodevelopment of babies and improve the outcome [16].
Hence, this study was planned to be conducted in the institute to determine various risk factors for neonatal hypoglycaemia and prevent hypoglycaemic episodes in neonates to decrease morbidity and improve neurological outcome in hypoglycemic neonates.
Materials and Methods
Study design and setting
A prospective observational health facility-based study was conducted in the Department of Pediatrics at a tertiary care hospital in Nagpur, Central India between November 2020 and November 2022 (24 Months).
Study participants
Neonates admitted in NICU with hypoglycaemia or who had hypoglycaemia during NICU stay.
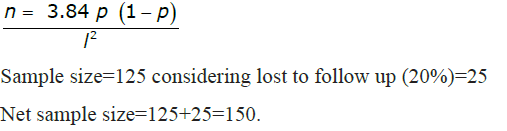
A sample size of 150 subjects, the sample size was calculated using a p=proportion of birth asphyxia in neonatal hypoglycaemia=43.39 (45) Level of confidence 95% l=error 20% of proportion formula
Exclusion criteria for cases
• New-borns with congenital malformation
• New-borns with suspected inborn errors of metabolism
• Maternal history of oral hypoglycemic agents, beta sympathomimetic drugs
Data collection
This is a prospective observational study in NICU of a tertiary Health Care Hospital of central India. For data collection babies satisfying inclusion criteria were enrolled in the study after taking written informed consent of mother or caregiver, from which Prevalence of hypoglycemia is calculated. High risk new born are screened for hypoglycemia since admission into NICU by point of care glucometer devices which use glucose oxidase-peroxidase method. Blood sugar ≤ 45 mg/dl taken as cut-off for hypoglycaemia. Screening for hypoglycaemia done at 2,4,6,12,24,28,72 hrs and then every 24 hrs up to 7 days of life in high-risk babies. Those who had low blood sugar, screening frequency was increased depending upon the blood sugar. Baseline variables and age at onset of hypoglycaemia are recorded. Asymptomatic hypoglycaemia with blood sugar 20-45 mg/dl treated with feeding. For symptomatic babies 10% Dextrose bolus followed by glucose infusion rate was started at 6 mg/kg/min. GIR was increased at 2 mg/kg/min depending upon the response upto a maximum of 12 mg/kg/min. If blood sugar is not maintained with Glucose Infusion Rate (GIR) fluid that corticosteroids are added and Octreotide is added if there is no response to steroids for 24 hours. Survival and duration of treatment required for hypoglycaemia is compared. Base line investigations were done as per needed on case-to-case basis.
Statistics analysis
All the data was entered into a well-designed MS Office Excel sheet and results were expressed in terms of number and percentage.
Ethical consideration
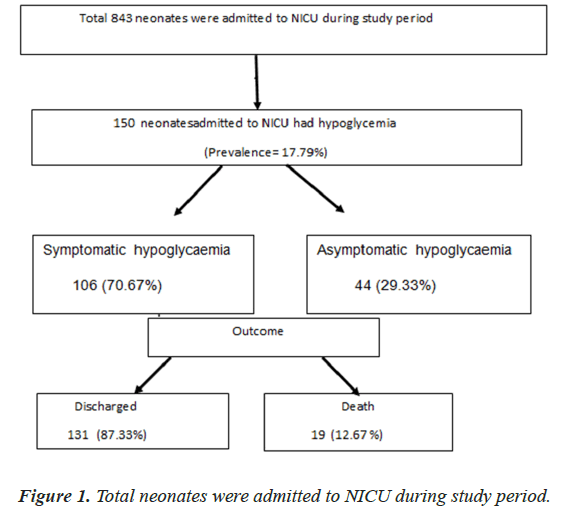
Ethical clearance for conducting the study was obtained from the institutional Ethics Committee. Information obtained during the study is confidential. A written informed consent in the local language from parents or guardians of each enrolled patient who were willing to get enrolled in the study after explaining to them the nature of the study (Figure 1).
Results
This prospective observational study was carried out in a NICU of a tertiary care centre over a period of 2 years. During study period, total 843 neonates were admitted to NICU and 150 neonates had hypoglycaemia. Prevalence of hypoglycemia was 17.79% in this study. Out of 150 neonates with hypoglycemia, 88 (58.67%) were male neonates and 62 (41.33%) were female neonates, showing male preponderance. Among 150 babies with neonatal hypoglycemia 58 (38.66%) were VLBW followed by 52 (34.67%) babies were LBW 28 (18.67%) were normal weight and 12 (8%) babies were ELBW babies. Out of 150 hypoglycemic neonates majority were preterm babies amounting 109 (72.67%) and 41 (27.33%) babies were full term. Hypoglycemia was more common in babies who were born preterm.
Table 1 shows relationship between neonatal hypoglycemia and maternal risk factors. Among the maternal risk factors PIH was found in 40 (26.67%) neonates, PROM in 36 (24%) neonates, IDM in 21(14%) neonates, APH in 10(6.67%) neonates. No maternal risk factor was found in 54 (36%) neonates with neonatal hypoglycemia.
| Maternal risk factor | Number (%) |
|---|---|
| IDM | 21 (14) |
| PIH | 40 (26.67) |
| PROM | 36 (24) |
| APH | 10 (6.67) |
| No maternal risk factors | 54 (36) |
Table 1: Relationship between neonatal hypoglycaemia and maternal risk factors.
Table 2 shows the relationship between the neonatal hypoglycemia and the neonatal risk factors. Among neonatal risk factors maximum number of babies had septicemia 51 (34%) followed by RDS in 46 (30.67%) babies, Birth asphyxia in 17 (11.33%), meningitis in 11 (7.33%) and twin gestation 9 (6%) in babies with neonatal hypoglycemia. No neonatal risk factor was found in 61 (40.66%) neonates with hypoglycemia
| Risk factor | Number (%) |
|---|---|
| Birth asphyxia | 17 (11.33) |
| RDS | 46 (30.67) |
| Septicemia | 51 (34) |
| Meningitis | 11 (7.33) |
| Twin gestation | 9 (6%) |
| None | 61 (40.66%) |
Table 2: Relationship between neonatal hypoglycaemia and neonatal risk factors.
Table 3 shows short term outcome in neonatal hypoglycemia in the present study. Out of 150 neonates with hypoglycemia, 131 (87.33%) babies were discharged from NICU and 19 (12.67%) babies with hypoglycemia died during NICU stay.
| Immediate outcome | Number (%) |
|---|---|
| Death | 19 (12.67) |
| Discharge | 131 (87.33) |
Table 3: Shows short-term outcome in neonatal hypoglycaemia
Among the 19 deaths, PROM (42.1%) was most common maternal risk factor followed by APH (31.57%), PIH (21.05%) and IDM (10.52%). 10.52% of neonatal deaths had both PIH and PROM as maternal risk factor.
Among the total 19 deaths, RDS (94.73%) was most common neonatal risk factor followed by septicemia (68.42%), Birth asphyxia (21.05%), Twin gestation (10.52%) and meningitis (0.052%).
Discussion
This was a prospective observational study, conducted in NICU of a tertiary care Hospital in central India over a period of 2 years.
The study was done to find out prevalence of hypoglycaemia, screening of high-risk neonates, to study clinical profile and maternal and neonatal risk factors neonatal hypoglycaemia. Total 843 neonates were admitted in NICU care during study period out of which 150 neonates had hypoglycaemia. Prevalence of hypoglycaemia in this study was 17.79% in NICU admitted babies.
Among 150 hypoglycaemic neonates 88 babies were male (58.67%) and 62 were female (41.33%). Among hypoglycemic neonates male neonates were more than female neonates (Male: female ratio 1.41:1). Similar findings were observed by Somanathan, et al. (M: F=1.65), Kumar et al., [17] (M: F=1.43), Gopchade [18] (M: F=1.4), Babu et al., [19] (M: F=1.35:1), Najati et al. [20] (M: F=1.2:1), and Kumar, et al. [21] found incidence of neonatal hypoglycemia in males (35%) was more than in females (31%). Choudhury, et al. [22] found incidence of hypoglycemia in males (35%) was more than the females (27.6%). Melana ,et al. [23] observed that among hypoglycemic babies males (69.2%) were more than females (30.8%). Anjum, et al. [24] (M: F=1.08) reported almost equal frequency of hypoglycemia in male and female neonates. On the contrary Stomnaroska, et al. [25] observed hypoglycemia in female was more than male neonates (M: F=0.72).
The present study PIH was found in 26.67% of hypoglycemic neonates as a most common maternal risk factor, similarly other studies also found PIH as common maternal risk factor including Manjunatha, et al. in 32.5%, Kallur, et al. [26] in 26.8%, Nishikant, et al. [26] in 24%, Anjum, et al. in 22%, Sasidharan, et al. [26] in 15.55%, Somanathan et al., in 14% and Ajeet Gopchade in 10% of hypoglycaemic neonates. In our study PROM was found in 24% of hypoglycemic babies it was also reported as major risk factor for hypoglycemia by Nishikant, et al. (16%), Gopchade (8.33%), Sasidharan, et al. (7.81%) and Somanathan, et al. PROM (0.9%). In this study maternal diabetes mellitus was reported as a maternal risk factor in 14% of hypoglycemic neonates while Tom et al., reported 42.6%, Nishikant, et al. reported 36%, Anjum, et al. reported 38%, Najati, et al. reported 13.6%, Somanathan, et al. reported 20.4%, Gopchade reported 18.33% and Sasidharan, et al. reported 6.25% of hypoglycemic neonates. APH was identified as maternal risk factor for hypoglycemia in 6.67% of hypoglycemic babies which was slightly higher than reported by Nishikant, et al. (4%) [27].
In present study, maximum babies had septicemia 51 (34%) followed by RDS in 46 (30.67%) babies, Birth asphyxia in 17 (11.33%), meningitis in 11 (7.33%) and twin gestation 9 (6%). In present study, 34% of hypoglycemic neonates had septicemia which was also reported as neonatal risk factor by Anjum, et al. (20%), Tiple, et al. (18.86%), Gopchade (13.33%), Najati et al. (9.6%) and Kallur et al. (4.8%). RDS was found in 30.67% of hypoglycemic neonates value closer to study done by Tiple et al. (29.24%) and Anjum et al. (31%). In our study Birth asphyxia was reported in 11.33% of hypoglycemic neonates which was less than reported by Tiple et al. (43.39%), Gopchade (26.67%) Kallur et al. (19.5%) but higher than reported by Najati et al. (9.6%). Somanathan et al. collectively reported sepsis, birth asphyxia, polycythaemia and shock in 16.3% of the hypoglycaemic neonates. Meningitis reported by Tiple et al. in 8.49% of hypoglycemic babies was slightly higher than reported in present study (7.33%) [28].
Out of 150 neonates with hypoglycemia 131 (87.33%) babies were discharged from NICU and 19 (12.67%) babies with hypoglycemia died. Mortality of 12.67% was found in the present study. Neonatal mortality in neonates with hypoglycemia reported by Tiple et al. was 17.9%. In our study majority were ELBW (47.37%) and 89.47% babies who died were having birth weight below 2.5 kg. 94.73% of babies who died were preterm. PROM was seen in 8 (42.1%) deaths as a most common maternal risk factor. RDS, septicemia and birth asphyxia were the most commonly identified neonatal risk factor among the babies died, found in 18 (94.73%),13 (68.42%) and 4 (21.05%) deaths. Meningitis was the least common neonatal risk factor found in 1 (0.052%) of death. Nishikant et al. found that among deaths, birth asphyxia (47.37%), RDS (21.05%), septicemia (15.79%) and meningitis (15.79%) were most commonly found neonatal risk factors. The most common causes of neonatal deaths were not due to hypoglycemia per se but due to co morbid conditions like birth asphyxia, extreme prematurity with respiratory distress syndrome and sepsis.
Conclusion
In this study, the prevalence of neonatal hypoglycemia was 17.79%. PIH was found to be the most common maternal risk factor and neonatal septicemia was the most common neonatal risk factor. Most of the babies with hypoglycemia were symptomatic and lethargy was the most common clinical presentation at the time of hypoglycemia. Majority of neonates were discharged with normal neurological status.
Limitations
This is a single centre study. The study group included only neonates admitted in NICU and not all neonates in the hospital, it underestimates actual prevalence of hypoglycaemia so the data may not represent the entire population. Long term outcome in these babies on follow up were not assessed in the present study.
References
- Adamkin DH. Neonatal hypoglycemia. Semin Fetal Neonatal Med 2017; 22(1): 36-41.
- Adamkin DH, Committee on Fetus and Newborn. Postnatal glucose homeostasis in late-preterm and term infants. Pediatrics 2011;127(3):e20103851.
- Lucas A, Morley R, Cole T. Adverse neurodevelopmental outcome of moderate neonatal hypoglycaemia. BMJ 1988; 297(6659):1304-8.
- Beard A, Cornblath M, Gentz J, et al. Neonatal hypoglycemia: a discussion. J Pediatr 1971;79:314-24.
- Anderson JM, Milner RD, Strich SJ. Effects of neonatal hypoglycaemia on the nervous system: a pathological study. J Neurol Neurosurg Psychiatry 1967; 30(4):295.
- Banker BQ. The neuropathological effects of anoxia and hypoglycemia in the newborn. Dev Med Child Neurol 1967; (5):544-50.
- Ogata ES. Carbohydrate metabolism in the fetus and neonate and altered neonatal glucoregulation. Pediatr Clin North Am 1986; 33(1):25-45.
- Koivisto M, Blanco‐Sequeiros M, Krause U. Neonatal symptomatic and asymptomatic hypoglycaemia: a follow‐up study of 151 children. Dev Med Child Neurol 1972; 14(5):603-14.
- FLUGE G. Clinical aspects of neonatal hypoglycaemia. Acta Paediatr Scand 1974; 63(6):826-32.
- Haworth JC, Coodin FJ, Finkel KC, Weidman ML. Hypoglycemia associated with symptoms in the newborn period. Can Med Assoc J 1963; 88(1):23.
- Schaefer-Graf UM, Rossi R, Bührer C, et al. Rate and risk factors of hypoglycemia in large-for-gestational-age newborn infants of nondiabetic mothers. Am J Obstet Gynecol 2002; 187 (4):913-7.
- Cole MD, Peevy K. Hypoglycemia in normal neonates appropriate for gestational age. Comparative Study 1994; 14(2) :118-20.
- Heck LJ, Erenberg A. Heck LJ, Erenberg A. Serum glucose levels in term neonates during the first 48 hours of life. Comparative Study 1987; 110 (1):119-22.
- Dhananjaya CD, Kiran B. Clinical profile of hypoglycemia in newborn babies in a rural hospital setting. Int J Biol Med Res 2011; 2(4):1110-4. [Crossref][Google Scholar][Indexed]
- Wickström R, Skiöld B, Petersson G, et al. Moderate neonatal hypoglycemia and adverse neurological development at 2–6 years of age. Eur J Epidemiol 2018;33: 1011-20.
- Soltesz G, Jenkins PA, Aynsley-Green A. Hyperinsulinaemic hypoglycaemia in infancy and childhood: a practical approach to diagnosis and medical treatment based on experience of 18 cases. Acta Paediatrica Hungarica. 1984; 25(4):319-32.
- Kumar U, Singh BB. To determine the clinical profile of hypoglycemia in newborn and to determine the prevalence of hypoglycemia among neonates admitted in NICU. EJMCM 2020;7(10):2020.
- Gopchade A. Risk factors and clinical features of neonatal hypoglycemia: a prospective study. Ann Int Med Den Res 2020; 6(1):PE24-PE27.
- Babu MR, D’Souza JL, Susheela C. Study of incidence, clinical profile and risk factors of neonatal hypoglycemia in a tertiary care hospital. Int J Pediatr Res 2016;3(10):753.
- Najati N, Saboktakin L. Prevalence and underlying etiologies of neonatal hypoglycemia. Pakistan journal of biological sciences. PJBS 2010;13(15): 753-6.
- Kumar TJ, Vaideeswaran M, Seeralar AT. Incidence of hypoglycemia in newborns with risk factors. Int J Contemp Pediatr 2018;5(5):1952-5.
- Choudhury S, Chakrabarti SK, Debbarma SK. Neonatal hypoglycemia revisited: Incidence and clinical profile in a tertiary center hospital of Tripura. Indian J Child Health 2019; 28:87-90.
- Melana N, Ahmed N, Soni RK, et al. Neurodevelopmental Outcome in Neonates with Hypoglycaemia and Associated Risk Factors: A Follow up Study. J Preg Child Health 2017; 4: 323.
- Anjum R, Anjum R, Qayum S. Neonatal hypoglycemia: risk factors and clinical profile. J Med Sci Clin Res 2019;7(2):1081-5.
- Stomnaroska O, Petkovska E, Jancevska S, et al. Neonatal hypoglycemia: risk factors and outcomes. Pril 2017; 38(1):97-101.
- Kallur M, Dasari B. Clinical profile of hypoglycemia among newborn babies in a private medical college and hospital. MedPulse Inter J Pediat. 2020; 13:24-27.
- Nishikant T, Milind K, Ravindra C, et al. Neonatal hypoglycemia in a tertiary care hospital. int med j 2015; 2(7): 419-423.
- Sasidharan CK, Gokul E, Sabitha S. Incidence and risk factors for neonatal hypoglycaemia in Kerala, India. Ceylon Med J 2010; 49(4).