Current Pediatric Research
International Journal of Pediatrics
Two years of premarital screening program for hemoglobinopathies in Karbala, Iraq; Outcome and options for improving the program.
Mohammed Naji Atiyah1*, Basheer Akeel Al –Ali2, Hassan Mousa Abd3
1Department of Pediatrics, Karbala hospital for Children, Hereditary Blood Disease Center, Karbala, Iraq
2Department of Pediatrics, University of Karbala College of Medicine, Karbala, Iraq
3Department of Pediatrics, Karbala hospital for children, Hereditary Blood disease center, Karbala, Iraq
- Corresponding Author:
- Mohammed NajiAtiyah
Department of Pediatrics
Karbala hospital for children
Hereditary blood disease center
Karbala
Iraq
Tel: 009647813088044
E-mail: alaaj.nasrawi@uokufa.edu.iq
Accepted date: May 26th, 2021.
Background: Thalassemia and sickle cell disease are common autosomal recessive disorders and are the most widespread single gene disorder that considered important public health problems. Premarital screening is important step in prevention of hemoglobinopathies.
Aim: to evaluate the outcome of 2 years of the premarital screening program in Karbala and options to improve that program.
Methods: A descriptive cross-sectional study by assessment of 2 years of premarital screening in Karbala Blood Disease Center started from January 2019 till December 2020. Total number of individuals screened for hemoglobinopathies in that period was 1306 (653 couples) referred from five marital clinics, Complete blood count was done for all screened couples.
Results: The bulk number of tested individuals was in 2019 because of the corona pandemic, nearly half of those couples were relatives, the majority was referred from Al-Husseini hospital, about 5% of these marriages were contraindicated to be accomplished and 3 % were cautious. β-Thalassemia minor was the main type of abnormal hemoglobinopathies discovered.
Conclusion: Some risky marriages were prevented by doing the premarital screening but still we need other concerted efforts to improve the outcome of the program.
Keywords
Premarital screening, Prenatal diagnosis, Hemoglobinopathies, Thalassemia, Sickle cell anemia.
Introduction
Thalassemia and sickle cell disease are common autosomal recessive disorders and the most widespread single gene disorders are considered important public health problems in Middle Eastern countries, including Iraq [1]. Hemoglobinopathies, including the hemoglobin variants and thalassemia, are groups of inherited disorders of Hemoglobin synthesis arising from mutations and/or deletions of one or more of the globin genes resulting in production of structural chains synthesis variants such as (Hemoglobinopathy S, Hemoglobinopathy C, Hemoglobinopathy E, and Hemoglobinopathy D) in the former and decrease rate of synthesis of structurally normal globin chains in the latter [2].
In spite of the carrier states of both conditions may be clinically unapparent, the homozygous or the doubly heterozygous states manifest clinically as anemia of varying degree of severity [3]. It is wise to remember that hemoglobinopathies are the most common single gene disorder worldwide [4]. More than 330000 affected infants are born in global manner yearly with 3.4% deaths in children less than 5 years [5]. β-Thalassemia is serious public health problem and it is wide spread throughout the region of Africa, the Mediterranean region and Middle East in which Iraq is located, Indian peninsula, and Southeast Asia [6]. As approximate estimate 3% of the world’s population carry genes for β-thalassemia [7]. The highest prevalence has been reported in Cyprus, Italy (Sardinia) and south Asia [8].
β-TM is encountered at different frequencies in almost all Arab countries with carrier rates of 1%-11%, and the frequency is higher in Jordan, Lebanon, Iraq, Egypt, Palestine, and other Arab countries [3]. In Iraq, the carrier rate of β -thalassemia in different governorates is rather uniformly distributed throughout the country, ranges between 3.7% and 6.5% [9], and with 15,000 registered patients with thalassemia major/ intermedia [10,11]. Sickle cell disorders, on the other hand, are less uniformly distributed with carrier rates varying from 0%- 16.0%, and they cluster especially in the south and north of the country [12].
These are relatively high carrier rates of autosomal recessive disorders coupled with nearly 24%-30% rates of consanguineous marriages in the population [13], while the prevalence of β-Thalassemia carrier in Karbala governorate is (3.8%). It was comparable to other regions of the country and the prevalence of sickle cell disease hemoglobin was obviously low 0.56%, which is not representing the true figure of sickle cell carriers in Karbala governorate [14] because there is no definitive cure for these hereditary diseases. Apart from bone marrow transplantation, which is expensive and risky; moreover, it is difficult to identify a suitable donor, and the required infrastructure is unavailable in most Middle Eastern countries, in addition the cost of blood transfusions for β- thalassemia major patients in the Middle East has been estimated approximately USD 3,200 annually per patient, with lifetime costs of approximately USD 284,145 [15], add the cost of chelating therapy which is again costly, for that the World Health Organization (WHO) has suggested a control program comprising culturing of the public, screening for carriers, prenatal diagnosis and genetic counselling, which would result in the prevention of the births of an affected children.
Italy, Greece, Canada, United Kingdom, and Cyprus started the program in the 1970’s and achieved success [16]. The high incidence of consanguinity among our populations plays a very important role in maintaining the recessive pattern of inheritance and increases the risk of homozygous or doubly heterozygous clinically affected offspring creating great psychological and financial stresses on the families and great burdens on the financial resources of many countries in the region.
Premarital screening for hemoglobinopathies is an important tool in the prevention process for these groups of hereditary disorders, combining with raising awareness and carrier screening in addition to prenatal and/or neonatal diagnosis assist in decreasing the escalating number of newly diagnosed patients in Karbala city/Iraq. Absence of molecular tools for the time being put extra efforts on the first three essential steps, frankly speaking there is dereliction regarding raising awareness and carrier screening, so premarital screening plays a pivotal rule in prevention of these disorders. As a step aiming at prevention of these diseases, in June 2012, the Department of Health in Karbala governorate established its “premarital screening program”. The premarital screening in Karbala hereditary blood disease center was principally designed to control β-thalassemia due to its high prevalence with the participation of five premarital clinics which is established in the five main hospitals of Karbala center and their main provinces.
Premarital screening Program and Genetic Counseling (PMSGC) in all over the governorates of the country together with Prenatal Diagnosis (PND) if possible, is the optimum choice to reduce the burden of β-thalassemia. For example, In Iran, the total costs of preventing 1 case of β-thalassemia were estimated at 100 USD, less than the cost of a single year of optimum support for a case of β-thalassemia [17]. Similar findings in Greece and Cyprus indicated that the cost of prevention was equal to that of treating one affected patient for one year, while the-annual cost of the screening program was equivalent to treating the thalassemia-affected population for 1 week [18].
Prevention thus appears to be significantly more cost effective while reducing the psychosocial implications of this chronic disease [19]. The aim of our study is to assess two years of premarital screening program, and their outcome and option for improving that outcome in reducing the birth of new cases of major hemoglobin disorders in Karbala.
Materials and Methods
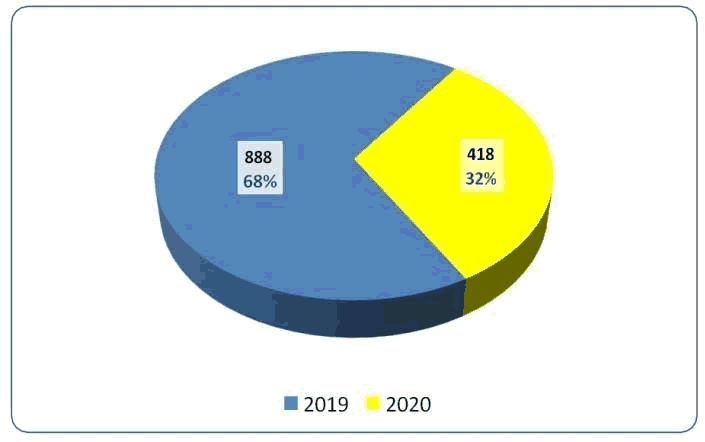
A descriptive cross-sectional study evaluating two years of premarital screening for hemoglobinopathies in Karbala, started from January till December, 1306 persons (653 couples) was registered in Karbala blood disease center in that period, 888 persons (444 couples) in 2019 and 418 persons (209 couples) in 2020. Obviously because of the impact of the Corona pandemic the number have almost halved in the second year of our survey. Five premarital clinics referred thosepeople according to a well-established guideline. These clinics located inside the main governmental hospital of the governorate, these are Al-Husseini general hospital, obstetric and gynecological hospital, Al-Hindiya general hospital, Al- Hussainya general hospital, Ain al-tamur general hospital.
Every couple applies for marriage certification is mandatorily required to visit their district hospital for premarital screening for hemoglobinopathy. Three milliliter (ml) venous blood sample is collected from each individual in EDTA tube.
Complete Blood Count (CBC) with differential count is done within 4 hours using Sysmex XN-350 blood cell auto analyzer, which is calibrated according to manual user advice every 100 samples. Men blood sample tested first because carrier woman in our community may be considered flaw and decrease her chances of marriage.
If the MCH was ≥ 27 pg., and the MCV was ≥ 80 fl., it would be safe completing marriage regarding hemoglobinopathy. If the man has MCV<80 fl., and/or MCH<27 pg., his partner woman blood sample should be tested for CBC. If the woman CBC was normal, the marriage is considered safe. If both man and woman have MCV<80 fl., and/or MCH<27 pg., they should be referred to Karbala hereditary blood diseases center to be tested for abnormal hemoglobin. In the center 5 ml venous blood sample collected to test for hemoglobin electrophoresis and serum ferritin. Hb-electrophoresis is done with Bio-Rad D10 automated HPLC system and occasionally by sebia capillary electrophoresis, which is calibrated systematically with kit replacement as recommended by operator.
Serum ferritin and exceptionally other tests like (serum iron, total iron- binding capacity, blood film, sickling test,etc.) and other necessary tests were done if needed to differentiate other causes of anemia. We depend on a suggestive clinical course in addition to the following well known criteria to verify the [20- 22] diagnosis:
• B-thalassemia trait, Hb A2 ≥ 4% and Hb F 0.1%-5%.
• B-thalassemia intermedia, the onset of clinical presentation usually after the age of 2 years, Hemoglobin level ~7 g/ dl- 10 g/dl, Hemoglobinopathy F 10%-50% may reach up 100% and Hemoglobin A2>4%.
• B-thalassemia major, the onset of clinical presentation usually before the age of 2 years [21], Hemoglobin level usually<7 g/dl, Hemoglobinopathy F up to 100% and Hemoglobin A2 is elevated.
• Possible α-thalassemia traits, Hemoglobin F<1% but sometimes variably elevated in the capillary method, Hemoglobin A2<2% plus microcytic hypochromic RBC (confirmed by DNA Study).
• Hemoglobinopathy E constitutes of 25%-30% of the total hemoglobin in hemoglobin E carrier, while in homozygous state Hemoglobin E reaches up to 85%-95% and Hemoglobin F 5%-10%.
• Structural Hemoglobin Variants like Hemoglobinopathy S, C and D this is achieved through HPLC. And/or capillary electrophoresis, if the pre-dominant Hb in the chromatogrm was abnormal then it is a disease status. We need S-Window<50% and Hb A>50% for diagnosis of sickle cell trait and if S-Window>50%, Hb A<50% for diagnosis of sickle cell disease.
• SB+ is confirmed if at least 50% of the Hb is Hemoglobinopathy S, Hb A is present in good quantity and the amount of Hb A2 is elevated (typically>3.5%) by capillary not by D-10 method, SBo is confirmed if at least 50% of the Hb is Hemoglobinopathy S, Hb A is not present and the amount of Hb A2 is elevated (typically >3.5%) by capillary not by D-10 method. So far if S-Window<50%, Hemoglobin A>50% and Hb A2>3.5% by capillary not by D-10 for diagnosis of sickle thalassemia trait or Hb ASF. Condition in the person to be tested, status termed as compound or double heterozygous state.
These rules applied to other structural hemoglobinopathies like Hemoglobinopathy D and C [23].
It was unpractical to do hemoglobin electrophoresis and sickling test to all screened couples. Screened couples were informed in details about the importance of steps done. Analysis of results and concluding the outcome of these marriages was clarified to couples in details. Certificate of hemoglobinopathy status supplied after signing and approval by three specialist working in the center and genetic counseling was provided especially if there was risky marriage and they were sent back to the referring premarital clinics but the decision to proceed in marriage or not was left to the couple themselves, those risky or cautious marriages were called back to inquire about the results of these marriages, The data of Karbala Blood Diseases Center was used to estimate the newly registered cases in these two years, couples signed written consent before they were enrolled in this study assuring confidentiality of results for all the participants.
Results
The total number of individuals examined during the study period (2019 and 2020) was 1306 participants. The mean age of couples at time of marriage was 22.25 ± 6.75 years, ranging from 13 to 73 years with no significant difference in mean age of couples in 2019 and 2020. The study revealed that about half of couples were relatives while the other half was strangers. Employed individuals accounted for less than half of the study population (43.7%) whereas unemployment accounted for only 1.8% with no significant difference in mean age of couples in 2019 and 2020. Less than two thirds of the study population (62.2%) was urban whereas rural about one quarter (26.6%) with no significant difference in means age of couples in 2019 and 2020 (Figure 1 and Table 1).
| Variables | Categories | Total No. (%) (n=1306) | 2019 No. (%) (n=888) | 2020 No. (%) (n=418) | P value | |
|---|---|---|---|---|---|---|
| Age (in years) | Mean ± SD | 22.25 ± 6.75 | 22.35 ± 6.90 | 22.04 ± 6.43 | 0.436 | |
| Range | 13-73 | 14-73 | 13-66 | |||
| Consanguinity | Relatives | 630(48.2) | 420(47.3) | 210(50.2) | 0.321 | |
| Strangers | 676(51.8) | 468(52.7) | 208(49.8) | |||
| Occupation | Employee | 571(43.7) | 382(43) | 189(45.2) | 0.242 | |
| Housewife | 478(36.6) | 325(36.6) | 153(36.6) | |||
| Student | 234(17.9) | 161(18.1) | 73(17.5) | |||
| Unemployed | 23(1.8) | 20(2.3) | 3(0.7) | |||
| Residence | Center of Karbala | Urban | 812(62.2) | 563(63.4) | 249(59.6) | 0.378 |
| Rural | 348(26.6) | 227(25.6) | 121(28.9) | |||
| OutsideKarbala | 146(11.2) | 98(11) | 48(11.5) | |||
Table 1: Socio-demographic characteristics of the study population.
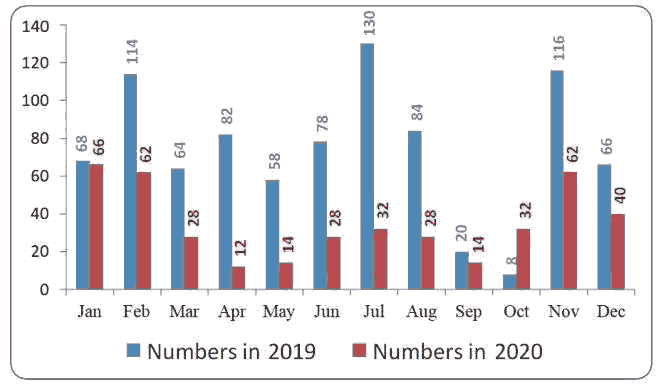
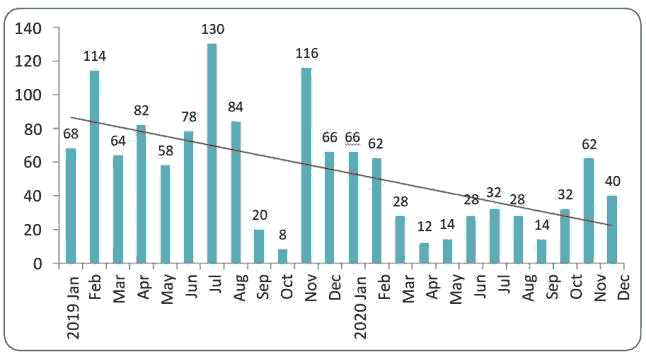
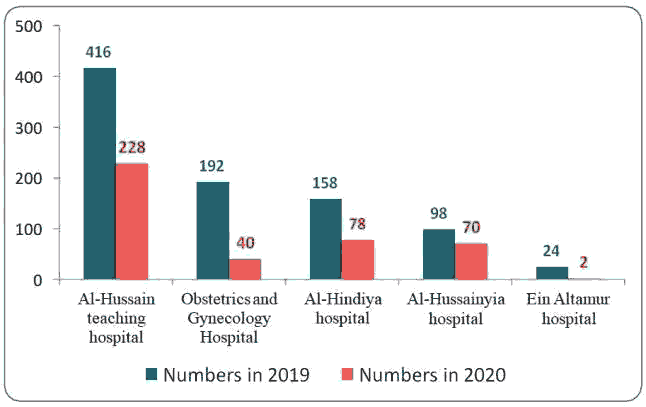
Figure 2 below showed the number of examined individuals each month of the two years under the study, Figure 3 revealed the down-slopping trend line in numbers through the months of the year 2019 to 2020.The results of the study also showed the number of individuals examined in each center which revealed that Al-Hosseini teaching hospital had the largest number of examinations as showed in Figure 4 below.
The results of laboratory examination of the study individuals showed that there were significant statistical differences in the Hb, MCH, MCHC and Hb A% levels among the two periods of the study (2019 and 2020) as showed in Table 2 below:
| Variables | 2019 (Mean ± SD) | 2020 (Mean ± SD) | P value |
|---|---|---|---|
| RBC | 5.31 ± 1.86 | 5.30 ± 0.75 | 0.979 |
| Hb | 12.34 ± 2.15 | 11.96 ± 1.93 | 0.002* |
| HCT | 37.32 ± 6.23 | 37.32 ± 5.76 | 0.99 |
| MCV | 71.36 ± 8.23 | 70.60 ± 7.10 | 0.104 |
| MCH | 23.61 ± 3.34 | 22.78 ± 2.81 | 0.0001* |
| MCHC | 32.73 ± 2.90 | 32.21 ± 2.09 | 0.001* |
| RDW | 15.42 ± 3.60 | 16.60 ± 17.80 | 0.059 |
| Iron | 54.28 ± 77.30 | 50.73 ± 69.97 | 0.425 |
| F | 1.17 ± 2.83 | 1.07 ± 2.02 | 0.609 |
| A2% | 2.96 ± 1.05 | 2.95 ± 1.23 | 0.937 |
| A% | 83.37 ± 7.33 | 91.34 ± 11.78 | 0.0001* |
Table 2:Laboratory investigations of the couples during the two years of the study.
The main abnormal Hemoglobinopathy diagnosed among refereed individuals was β-Thalassemia minor according to Table 3.
| Diagnosis | No. of affected individuals in 2019 | No. of affected individuals in 2020 | Percentage of the 2 years |
|---|---|---|---|
| ß-thalassemia minor | 114 | 73 | 187 (77.6%) |
| ß-thalassemia intermedia | 2 | 0 | 2 (0.8%) |
| Hb AS. | 28 | 12 | 40 (16.6%) |
| Hb AD. | 3 | 2 | 5 (2.074%) |
| Hb ASD. | 1 | 0 | 1 (0.4%) |
| Hb AC. | 1 | 0 | 1 (0.4%) |
| Hb D ß+thalassemia | 0 | 1 | 1 (0.4%) |
| Hb E disease | 0 | 1 | 1 (0.4%) |
| dß thalassemia | 0 | 2 | 2 (0.8%) |
| Abnormal Hb. variant need to be confirmed | 0 | 1 | 1 (0.4%) |
Table 3: Abnormal Hb among referred individuals.
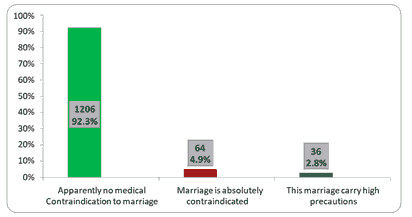
Regarding the medical contraindication to marriage 92.3% of them apparently had no medical contraindication to marriage regarding hemoglobinopathies, 4.9% marriage was absolutely contraindicated and 2.8% marriage carried high precautions as illustrated in Figure 5 below.
There were no statistically significant differences regarding contraindication to marriage among relatives and strangers, the year 2019 and 2020 and urban versus rural population (p>0.05). Whereas there were statistically significant differences of contraindication to marriage in relation to referring hospital (p=0.008) (Tables 4-7).
| Independent variables | Contraindication: No. (%) | P value | ||
|---|---|---|---|---|
| No medical contraindication (N=1206) | Contraindicated or precaution (N=100) | |||
| Year | 2019 | 824(92.8) | 64(7.2) | 0.373 |
| 2020 | 382(91.4) | 36(8.6) | ||
| Referring Hospital | Al-Hussain teaching hospital | 594(92.2) | 50(7.8) | 0.008* |
| Obstetrics and gynecology hospital | 210(90.5) | 22(9.5) | ||
| Al-Hussainyia hospital | 156(92.9) | 12(7.1) | ||
| Al-Hindiya hospital | 226(95.8) | 10(4.2) | ||
| Ein Al-tamur hospital | 20(76.9) | 6(23.1) | ||
| Relationship | Relatives | 576(91.4) | 54(8.6) | 0.23 |
| Strangers | 630(93.2) | 46(6.8) | ||
| Residence | Urban | 752(92.8) | 58(7.2) | 0.56 |
| Rural | 316(91.9) | 28(8.1) | ||
| Outside Kerbala | 132(90.4) | 14(9.6) | ||
Table 4: Contraindication to marriage regarding hemoglobinopathies and their relation to certain variables.
| Cautious marriages in 2019 | Cautious marriages in 2020 | Percentage | ||
|---|---|---|---|---|
| Fate of cautious marriages | No. of couples | Fate of cautious marriages | No. of couples | 22 couples |
| Not reached | 8 | Not reached | 2 | 10 (45.45%) |
| Cancelled | 1 | Cancelled | 0 | 1(4.5%) |
| Planning to marry | 0 | Planning to marry | 1 | 1 (4.5%) |
| completed the marriage | 7 | completed the marriage | 3 | 10(45.45%) |
| Sum | 16 | Sum | 6 | 22 |
Table 5: Details of cautious marriages in 2019-2020.
| Contraindicated to marry in 2019 | Contraindicated to marry in 2020 | Percentage | ||
|---|---|---|---|---|
| Fate of contraindicated marriages | No. of couples | Fate of contraindicated marriages | No. of couples | 32 couples |
| Not reached | 3 | Not reached | 4 | 7(21.8%) |
| Cancelled | 6 | Cancelled | 2 | 8(25%) |
| Already married | 2 | Already married | 1 | 3(9.37%) |
| Married | 7 | Married | 7 | 14(43.75%) |
| Sum | 18 | 14 | 32 | |
Table 6: Details of contraindicated marriages in 2019-2020.
| Cases | No. of cases in 2019 | No. of cases in 2020 | Percentage of 2 years |
|---|---|---|---|
| The marriage done before the program | 11 | 9 | 20 (39.2%) |
| The patient is transferred from another governorate | 7 | 4 | 11 (21.5%) |
| Produced an affected baby in spite of being having previous affected one | 4 | 2 | 6 (11.7%) |
| Did the premarital tests and given the proper counselling, yet married and produced affected child | 1 | 3 | 4 (7.8%) |
| Married without doing the requested premarital tests | 2 | 2 (3.9%) | |
| Did the premarital tests and not informed about the risk (as claimed) | 3 | 3 (5.8%) | |
| Structural Hb. disorder and difficult to detect the carrier state in the parents | 1 | 1 (1.9%) | |
| Parents of child not reached | 4 | 4 (7.8%) | |
| Sum | 33 | 18 | 51 |
Table 7: Registered cases in Karbala hereditary blood disease center in 2019-2020 in correlation with premarital screening for hemoglobinopathies.
Also, we have registered 52 cases of sickle cell anemia in 2019 and 26 cases on 2020 in addition to 9 cases of Hemoglobinopathy H disease in 2019 and 4 in 2020, most of them are adolescents and adults, those in the vast majority of cases are products of marriages before the premarital screening program implementation and actually reflect the improvement in diagnosis facilities inside the center.
Discussion
During the research period we had been examined 653 couples for screening of hemoglobin disorders, 444 couples in 2019 and 209 in 2020. The number of screened populations is almost halved in the second year of the study because of the corona pandemic and its devastating consequences, also there is seasonal drop of marriage contracts during Moharram and Safar Arabic months which coincide with September and October in the period of the study, it is attributed to religious and social believes among Shiite population. AL Hussein teaching hospital referred the largest number of populations because it is the main hospital of the city while Ain Al-tamur hospital referred the smallest number of populations because of high level of endogamy and closed tribal society which put priority to clerk marriage contract rather than the official one in spite of the high carrier rate of hemoglobinopathies among the people of that region [14].
Almost half of the marriage attendees are relatives and up to 62% came from urban area while 11% of them are from other governorates. The statistical difference between 2019 and 2020 in the laboratory results carry no clinical significance and cannot be explained regarding Hb, MCH, MCHC. But for Hb A% the higher values in 2020 are attributed to the more reliance upon capillary electrophoresis in calculation of Hb A% rather than the variant 1 HPLC. In 2019, 241 out of 1306 carry abnormal Hemoglobin. (18.45%), in comparison to 25.3% abnormal Hemoglobin found in the same center in a previous study [14], of those 241, 187 (77.6%) have thalassemia minor and 40 (16.6%) have Hemoglobin AS., this is also to be compared to (81.5%) and (11.9%) for thalassemia minor and sickle cell trait respectively in the same study [14].
% of the referred individuals have thalassemia trait while 3.06% have Hemoglobin AS and 0.38% have Hemoglobin AD. Variant, while it was 20.6% for thalassemia minor, 3.01% for sickle cell trait and 0.83% for Hemoglobin AD. In the previous study in Karbala blood disease center (14), the rest have rarer hemoglobinopathy disorders, the lower incidence of hemoglobinopathies diagnosed in this study as compared to the previous one may be explained on the base of the smaller sample size, the main results were distributed between thalassemia trait and sickle cell trait, which is comparable to the reported prevalence rates of ß-thalassemia and sickle cell genes among Iraqi population [24]. Around 5% of these marriages are absolutely contraindicated because of the risk of reproducing Major Hb. disorder in their offspring while around 3% are cautious marriage, these considered as such due to many reasons, some of those couples not finished their tests and they did not come back to the center, some have borderline Hemoglobin A2 (3.2-3.8) with minor Hemoglobin disorder in the other mate, these all considered as cautious marriages and some of them might be silent carrier [25].
As shown in this study, the main bulk of those attending for premarital screening proceed to finish their project and only 25% of the contraindicated group and 4.5% of the cautious group decided to separate after being counseled. The reasons for such high rates of those proceeding with their marriage plans, which were also reported following premarital carrier screening programs in Saudi Arabia [26,27] are mainly due to social and cultural obligations and commitments as the premarital screening is performed only a few days prior to the actual legal ceremony.
In spite of the detailed genetic counseling provided, around 53% of the risky group completed marriage and some produced children, this is noticed in Islamic countries in general, for example In some regions of Iran there are strong cultural differences, in which, when a man chooses a woman as his wife and the family prepares for the ceremony, changing of decision is almost equal to getting divorced, so some couples could not separate at the time of diagnosis after both were found to be carriers [28].
In Iraq, generally the arrangements for marriage begins with the wedding which start after clerks decrees then after a period the governmental contract may or may not be performed, so by that time a lot of risky mattings might passed unnoticed or discovered lately, also the nearly absence of awareness among the population about hemoglobinopathies in spite of the big burden of these disorders and the high prevalence rate of β-thalassemia minor in Karbala, 3.8% which is comparable with those reported from Baghdad (4.4%) [29], Basra (4.6%) [30], Dohuk (3.7%) [31], but higher than those reported in neighboring countries like Lebanon (1.7%-3%) [29], Saudi Arabia (3%) [32], but the Iranian figures on the other hand is higher than ours (5%-10%) [33]. All these factors play an important role in that issue, moreover the decision of marriage completion is left to couples themselves and there are no laws to forbid such mattings.
The main outcome for this program is prevention of birth of children affected with major Hemoglobinopathy disorder, and in correlation with the newly registered cases in Karbala hereditary blood disease center which not necessarily reflect the marriages in the study period, we saw that 39% of parents of registered cases married before the institution of the program which had been started in June 2012 in the governorate while 21.5% of the registered patients transferred from other governorates where the premarital tests panel not include hemoglobinopathies and this explain the importance of application of the program in all over the country.
Around 8% of parents of registered cases in the study period actually did the premarital tests in our center and given the proper genetic counseling, yet married and produced affected children. But overall, the total number of newly registered cases in Karbala blood disease center is halved in 2020 as compared to 2019 and we hope more decrease in the new births of major Hemoglobinopathy disorders in the coming years.
Conclusion
Premarital screening is important step in the prevention of hemoglobinopathies, but it is not enough alone to get rid of these cumbersome groups of disorders, a lot of efforts needed to reach to zero case diagnosis.
Recommendations
• We need the program to be implemented in the other governorates.
• Raising awareness all over the country about the presence of these diseases.
• Implementation of carrier detection programs or at least the cascade carrier screening which is very important to set those people capable of reproducing cases.
• Establishment of molecular clinics i.e., prenatal diagnosis and pre-implantation genetic diagnosis to give more flexibility and other options for those wishing to proceed in marriage in addition to facilitating bortions of affected fetuses (fatwa) and law maker legislations, all are options to improve the program and prevention of hemoglobinopathies in Karbala and in Iraq as a whole.
References
- Hamamy HA, Al-Allawi NA. Epidemiological profile of common haemoglobinopathies in Arab countries. J Community Genet 2013; 4(2):147-67.
- Wheatherall DJ, Clegg JB. The thalassemia syndromes. (4th edn) Blackwell Science Ltd, UK, USA, Australia. 2001.
- Lukens JN. The abnormal hemoglobins: General principles. (10th ed) Wintrobe's Clinical Hematology, Williams and Wilkins, Baltimore. 1999.
- Goonasekera HW, Paththinige CS, Dissanayake VHW. Population screening for hemoglobinopathies. Annu Rev Genom Hum Genet 2018; 19:355-80.
- Modell B, Darlison M. Global epidemiology of haemoglobin disorders and derived service indicators. Bull World Health Organ 2008; 86(6):480-7.
- Lo L, Singer ST. Thalassemia: current approach to an old disease. Pediatr Clin North Am 2002; 49(6):1165-91.
- Baghianimoghadam MH, Sharifirad G, Rahaei Z, et al. Health related quality of life in children with thalassaemia assessed on the basis of SF-20 questionnaire in Yazd, Iran: a case-control study. Cent Eur J Public Health 2011; 19(3):165-9.
- Cao A, Galanello R. Beta-thalassemia. Genetics in medicine 2010; 12(2):61-76.
- Alnakshabandi AA, Muhammad HA. Prevalence of β- Thalassemia carriers among a cohort of university students in Hawler Province of Iraqi Kurdistan. Iraqi J Pharm Sci 2009; 18(2):15-9.
- Yahya HI. Thalassaemia genes in Baghdad, Iraq. East Mediterr Health J 1996; 2(2):315-9.
- Hassan MK, Taha JY, Al Naama LM, et al. Frequency of haemoglobinopathies and glucose-6-phosphate dehydrogenase deficiency in Basra. East Mediterr Health J 2003; 9(1-2):45-54.
- Alkasab FM, Al-Alusi FA, Adnani MS, et al. The prevalence of sickle cell disease in Abu-AL-Khasib district of southern Iraq. J Trop Med Hyg 1981; 84(2):77-80.
- Tadmouri GO, Nair P, Obeid T, et al. Consanguinity and reproductive health among Arabs. Reprod Health 2009; 6(1):1-9.
- Attiyah MN, Al-Najafi WK. Original Paper Premarital Screening Program for Hemoglobinopathies in Karbala, Iraq. J Med 2020; 13(1):2293-300.
- Lahiry P, Al-Attar SA, Hegele RA. Understanding beta- thalassemia with focus on the Indian subcontinent and the Middle East. Open Hematol J 2008; 2(1):5-13.
- Cao A, Pirastu M, Rosatelli C. The prenatal diagnosis of thalassaemia. Br J Haematol 1986; 63(2):215-20.
- Ahmadnezhad E, Sepehrvand N, Jahani FF, et al. Evaluation and cost analysis of national health policy of thalassaemia screening in West- Azerbaijan province of Iran. Int J Prev Med 2012; 3(10): 687-92.
- Oseroff B. The Ethics of Prevention: Counselling, Consanguinity, and Premarital Testing for Beta-Thalassemia in Jordan. Princeton, Princeton University, Iran. 2011.
- SattariM, SheykhiD, Nikanfar A, et al. The financial and social impact of thalassemia and its treatment in Iran. Pharm Sci 2012; 18(3):171-6.
- Cappellini MD, Cohen A, Porter J, et al. Guidelines for the management of Transfusion Dependent Thalassaemia (TDT). (3rd edn) Nicosia (CY): Thalassaemia International Federation. 2014.
- Cappellini MD, Cohen A, Eleftheriou A, et al. Guidelines for the clinical management of thalassaemia. (2nd Revised edn) Nicosia (CY): Thalassaemia International Federation. 2008.
- DeBaun M, Frei-Jones M, Vichinsky E, et al. Nelson textbook of pediatrics. (20th edn) Elsevier, Philadelphia. 2016.
- Bain BJ. The alpha, beta, delta and gamma thalassaemias and related conditions. Haemoglobinopathy diagnosis.(2nd Edn) Wiley-Blackwell. Oxford, London, UK. 2006.
- Al Allawi NA, Al DouskyAA. Frequency of haemoglobinopathies at premarital health screening in Dohuk, Iraq: implications for a regional prevention programme. East Mediterr Health J 2010; 16 (4):381-5.
- Belhoul KM, AbdulrahmanM, Alraei RF. Hemoglobinopathy carrier prevalence in the United Arab Emirates: first analysis of the Dubai Health Authority premarital screening program results. Hemoglobin 2013; 37(4):359-68.
- AlHamdan NA, AlMazrou YY, AlSwaidiFM, et al. Premarital screening for thalassemia and sickle cell disease in Saudi Arabia. Genet Med 2007; 9(6):372-7.
- Al SulaimanA, Saeedi M, Al Suliman A, et al. Postmarital follow‐up survey on high-risk patients subjected to premarital screening program in Saudi Arabia. Prenat Diagn 2010; 30(5):478-81.
- Karimi M, Jamalian N, Yarmohammadi H, et al. Premarital screening for β-thalassaemia in Southern Iran: Options for improving the programme. J Med Screen 2007; 14(2): 62-6.
- Yahya HI. Thalassaemia genes in Baghdad, Iraq. East Mediterr Health J 1996; 2(2):315-319.
- Hassan MK, Taha JY, Al Naama LM, et al. Frequency of haemoglobinopathies and glucose-6-phosphate dehydrogenase deficiency in Basra. East Mediterr Health J 2003; 9(1-2):45-54.
- Al-Allawi NAS, JubraelJMS, AnwarA, et al. Service indicators from a regional hemoglobinopathy preventive program in Duhok-Iraq. In Proceedings of the 2nd pana Arab human genetics conference, Dubai, CAGS. 2007.
- El-Hazmi MA, Warsy AS. Appraisal of sickle-cell and thalassaemia genes in Saudi Arabia. East Mediterr Health J 1999; 5(6):1147-53.
- Karimi MEHRAN, Rasekhi AR. Efficiency of premarital screening of beta-thalassemia trait using MCH rather than MCV in the population of Fars Province, Iran. Haematologia 2002; 32(2):129-34.