Current Pediatric Research
International Journal of Pediatrics
To study the desaturation events, apneic episodes and success rate of nasal prongs and oxygen hood in reversal of CPAP in pre-term babies in neonatal intensive care unit.
Mahaveer Singh Lakra1*, Bhavana Lakhkar2, Sagar Ajayrao Karotkar2, Ashwini Lakra1, Amar Taksande1
1Department of Pediatrics, Jawaharlal Nehru Medical College, Datta Meghe Institute of Higher Education Research, Sawangi Meghe, Wardha, Maharashtra, India
2Department of Neonatology, Jawaharlal Nehru Medical College, Datta Meghe Institute of higher education research, Sawangi Meghe, Wardha, Maharashtra, India
- Corresponding Author:
- Mahaveer Singh Lakra
Department of Pediatrics,
Jawaharlal Nehru Medical College, Datta Meghe Institute of Higher Education Research,
Sawangi Meghe, Wardha, Maharashtra,
India
E-mail: lakra.mahaveer@gmail.com
Received: 25-Apr-2023, Manuscript No. AAJCP-23-97016; Editor assigned: 27-Apr-2023, AAJCP-23-97016 (PQ); Reviewed: 11-May-2023, QC No. AAJCP-23-97016; Revised: 01-Aug-2023, Manuscript No. AAJCP-23-97016 (R); Published: 08-Aug-2023, DOI:10.35841/0971-9032.27.8.1982-1987
Background: The Continuous Positive Airway Pressure machine (CPAP) has revolutionalized the management in neonatal intensive care units. Nasal prongs and oxygen hoods are the standards of care for giving oxygen to babies in the NICU. Regarding the optimal timing and method of weaning from CPAP, there are no specific guidelines.
Objectives: This study aims at analysis of desaturation events, apneic episodes and success rate of two oxygen delivery devices: Nasal prongs and oxygen hood after weaning and reversal of CPAP in preterm babies.
Methods: All stable preterm babies weighing <37 weeks who are weaned off from CPAP were included. The study was conducted in tertiary care NICU in a rural medical college Sawangi Meghe, Wardha, Maharashtra. It was a cross sectional, comparative study done over 9 months with a sample size of 92 babies.
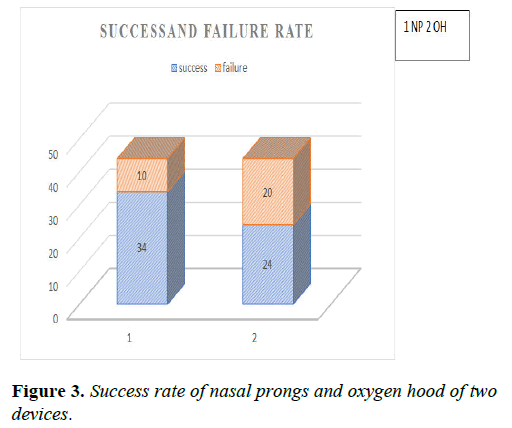
Results: The male to female ratio was 1.44:1. There was no statistical difference in the initial distribution of babies in the two groups (p-value 0.946). The incidences of early desaturations were more in the nasal prongs group as compared to the oxygen hood group (p-value<0.05). The episodes of severe desaturation (SpO2<85%) in the first 24 hours were more commonly seen with nasal prongs while mild desaturation episodes were equal in both groups (p-value 0.479). The apneic episodes were less with nasal prongs. The success rate with nasal prongs and oxygen hood was found to be 77.27% and 54.54% respectively which is statistically significant (p-value<0.05). The most common underlying cause for the restart of CPAP was desaturation.
Conclusion: The success rate of nasal prongs and oxygen hood was 77.27% and 54.54% respectively. Oxygen hood is better in the prevention of desaturation.
Keywords
New-born, Nasal prongs, Oxygen hood, Pulse oximetry, CPAP, Hypoxia
Introduction
Continuous Positive Airway Pressure (CPAP) is one of the most widely used modalities in the care of new-born babies [1]. Various proven methods of giving oxygen therapy in new-borns are oxygen hood, nasal prongs, nasopharyngeal catheters and giving oxygen from distance. The two most familiar methods are being commonly used are nasal prongs and oxygen hood [2]. The efficacy, episodes of desaturation, apnea and nasal injuries varies with both devices. Hyperoxia and hypoxia both are harmful to pre-term babies, so frequent fluctuation of FiO2 and SpO2 should be avoided [3]. It has always been a topic of debate that out of these two devices, which one to choose while weaning off from CPAP and during the recovery phase? Both devices have got their advantages and disadvantage in terms of desaturation, apnoeic episodes, nasal injury, cost effectiveness and acceptance [4]. Our approach should be saturation targeted in new-born preterm babies as unnecessary high oxygen exposure for a prolonged duration may lead to free radical injuries like retinopathy of prematurity, bronchopulmonary disease and other organ damage especially in vulnerable pre-term babies [5]. Very limited data are available on the efficacy of these two devices. A study done by Yllescas, et al. has shown that nasal prongs are better than oxygen hoods in the prevention of apneic episodes but inferior in terms of nasal injuries [6]. Studies done by Traver, CP et al. on environmental vs. nasal cannula supplemental oxygen for preterm infants and by Hensey CC, et al. on air or oxygen via nasal cannula to prevent desaturation in preterm infants showed different results with different modes [7,8]. There are no standard selection criteria for these two devices and the decision is taken merely by the treating neonatologist as per his/her acumen and it varies from one canter to other. This is the unique type of study that was conducted in India. Our study is unique as it takes into consideration the manual mode of oxygen hood and nasal prongs which are being widely used in almost all developing countries and is a standard of care in all neonatal ICUs world-wide [9-11].
PICO format
• Population: All preterm neonates <37 weeks in the process
of weaning from CPAP.
• Intervention: Nasal prongs for oxygen delivery.
• Comparison: Oxygen hood during weaning process.
• Outcome: Desaturation episodes and success rate.
Materials and Methods
This main aim and objectives was to study the episodes of desaturation, apneic episodes and success rate of nasal prongs and oxygen hood while reversal of CPAP after weaning in preterm babies. All stable preterm babies weighing <37 weeks who are weaned off from CPAP were included and put on oxygen therapy by any of the two modes. Exclusion criteria babies with choanal atresia, major congenital malformation and babies suffering from congenital muscular weakness. This study was conducted at tertiary care NICU in a rural medical college Sawangi Meghe, Wardha, Maharashtra which was a prospective, cross sectional, comparative study.
Total cases enrolled (n=92), excluded: n=2 (did not give consent), n=1 (LAMA), n=1 congenital anomaly, total babies study were 88.
The success rate of the device was determined by no increase in work of breathing/respiratory distress and episodes of desaturation, hemodynamically stable on an oxygen device and not requiring CPAP again.
Methods and statistical analysis: After putting on oxygen support by either means baby was continuously monitored by pulse oximetry for 96 hours for any desaturation/distress/apnoea. All demographic and clinical details were entered in a pre-tested and pre-validated format. Statistical analysis was performed by STATA software. Continuous variables are presented as means ± SDs, and categorical variables are given as frequencies with percentages. To compare continuous variables the student’s t-test was applied. The Chi square test was applied and p values <0.05 was considered significant.
Results
There was a total of 52 males and 36 females in our study and the male to female ratio was 1.44:1. Total of 11 (12.50%) babies were below the gestation of <28 weeks while 49 (55.56%) were between 29-32 weeks of gestation. The maximum 43 babies were in the birth weight group of 1.5 kg to 2.5 kg and a total of 9 babies were under 1000 gm of the birth weight. We calculated the mean weight and standard deviation for both gender in both groups. The mean birth weight for the male was 1650.29 ± 392 gm and 1637.16 ± 462.16 gm and for females 1419 ± 371.9 gm and 1691 ± 445.3 gm respectively in nasal prongs and oxygen hood group. The overall mean weight in nasal prongs and oxygen hood was 1566.13 ± 371 gm and 1661.70 ± 450 gm respectively.
The incidences of early desaturations were more in the nasal prongs group (37) as compared to the oxygen hood group (26) and were statistically significant (p value<0.05). More than 3 episodes of early desaturation were more commonly seen in the nasal prongs group (13.63%) as compared to hood group (6.83%). These episodes were transient and were not requiring a restart of CPAP. The multiple episodes >3 was more common in nasal prongs (18.18% vs. 6.81%) which were statistically significant (p-value 0.0293) as shown in Table 1.
| Episodes of desaturation | Nasal prongs | Oxygen hood | P-value |
|---|---|---|---|
| Early (within 24 hours) | |||
| No episode | 7 (15.90) | 18 (40.90) | 0.01144 |
| 1 episode | 17 (38.63) | 12 (27.27) | |
| 2 episodes | 14 (31.81) | 11 (25.00) | |
| 3 episodes | 6 (13.63) | 3 (6.83) | |
| Late (25-96 hours) | |||
| No episode | 13 (29.54) | 26 (59.09) | 0.02931 |
| 1 episode | 9 (20.45) | 8 (18.18) | |
| 2 episodes | 14 (31.81) | 7 (15.90) | |
| 3 episodes | 8 (18.18) | 3 (6.83) | |
Table 1. Distribution of patients according to the episodes of desaturation.
We also studied the severity of episodes of desaturation among both groups with respect to timings: Early or late as shown in Table 2.
| Level of desaturation | Nasal prongs n (%) | Oxygen hood n (%) | Total patient n (%) | P-value |
|---|---|---|---|---|
| Early desaturation in 24 hours | ||||
| No desaturation | 10 (22.72%) | 16 (36.36) | 26 (29.54) | 0.479 |
| SpO2 <85% | 10 (22.72) | 6 (13.63) | 16 (36.36) | |
| SpO2 86%-90% | 15 (34.09) | 14 (31.81) | 29 (32.85) | |
| SpO2 91%-95% | 9 (20.45) | 8 (18.18) | 17 (19.81) | |
| Late desaturation (25-96 hours) | ||||
| No desaturation | 23 (52.27) | 26 (59.09) | 49 (55.68) | 0.888 |
| SpO2 <85% | 6 (13.63) | 4 (9.09) | 10 (11.36) | |
| SpO2 86%-90% | 10 (22.72) | 9 (20.45) | 19 (21.59) | |
| SpO2 91%-95% | 5 (11.36) | 5 (11.36) | 10 (11.36) | |
| Total | 44 | 44 | 88 | |
Table 2. Distribution according to the early and late severity of desaturation and oxygen saturation.
The episodes of severe desaturation (SpO2<85%) in first 24 hours were more commonly seen with nasal prongs 10 (22.72%) than oxygen hood in 6 (13.63%). There was no statistical difference in the severity of late events of desaturation in nasal prongs and oxygen hood group (p value 0.888). The overall serious episodes of desaturation SpO2<85% were more commonly seen in a greater number of patients in nasal prongs groups (16) patient as compared to oxygen hood (10) however, this value was not statistically significant.
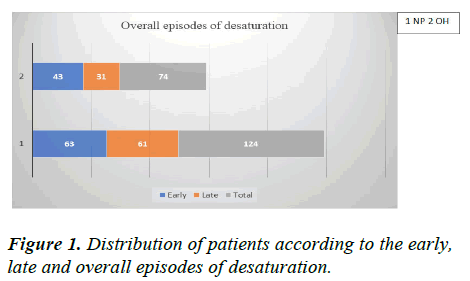
When we compared the overall events of desaturation between 2 groups, there were total 124 (60.48%) episodes in nasal prongs group and 74 (36.09%) episodes in oxygen hood. The early (63) and late (61) were more common with nasal prongs as compared to oxygen hood (43 vs. 32) but they were not statistically significant (p value 0.318) as shown in Figure 1.
The total 12 (27.27%) patients in nasal prongs group while 18 (40.91%) in hood group developed early apneic episodes. The late apnoeic episodes were also almost equally distributed (14 vs. 16) in two groups and they were not statistically significant (p value>0.05) as shown in Table 3.
| Apneic episodes | Nasal prongs n (%) | Oxygen hood n (%) | Total | P-value |
|---|---|---|---|---|
| Apneic episodes in 24 hours | ||||
| Absent | 32 (72.72) | 26 (59.09) | 58 (65.90) | 0.177 |
| Present | 12 (27.27) | 18 (40.91) | 30 (35.22) | |
| Apneic episodes in 25-96 hours | ||||
| Absent | 30 (68.18) | 28 (63.64) | 58 (65.90) | 0.653 |
| Present | 14 (31.82) | 16 (36.36) | 30 (35.22) | |
| Total | 44 | 44 | ||
Table 3. Distribution of patients according to the apneic episodes as per the timings of presentation.
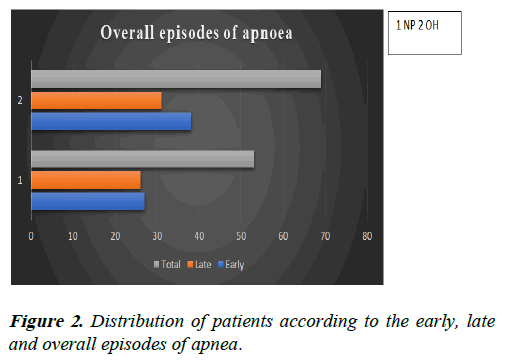
The total no of apneic episodes was less in nasal prong groups 53 (43,44%) as compared to oxygen hood 69 (56.55%). The early episodes were also less with nasal prongs 27 (41.53%) as compared to more with oxygen hood 38 (56.46%) however, the apneic episodes in both the groups individually and collectively were not statistically significant ( p value >0.05) as shown in Figure 2.
We analysed the need of restart of CPAP in both groups and it was seen that total 10 patients required CPAP in nasal prongs group while 20 patients required in oxygen hood group. The success rate with nasal prongs and oxygen hood was found to be 77.27% and 54.54% respectively which is statistically significant (p value<0.02452) as shown in Figure 3.
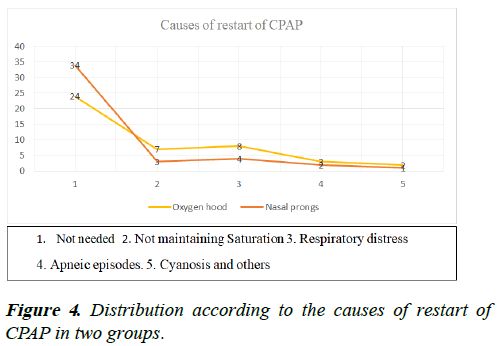
The overall common underlying causes for restart of CPAP have been depicted in Figure 4. The causes in both groups were almost similar as shown in table and these were not statistically significant.
Early CPAP<12 hours was need to be started in oxygen hood environment in 9 (20.45%) as compared to nasal prongs group 2 (4.54%).
Discussion
Total 88 babies were analysed, 44 being in each group. The overall male to female ratio in our study was 1.44:1. The results were comparable to other studies like Yllescas, et al. and Travers CP, et al. where male predominance was found. The mean gestational age in nasal prongs was 32.0 ± 2.4 weeks and in oxygen hood 34.4 ± 3.2 weeks respectively. A similar study done by travers CP, et al, and Yllescas, et al. had mean gestational age 27 ± 2 weeks 31.4 ± 2.7 and 31.2 ± 2.1 weeks in nasal prongs and hood group respectively.
The overall average weight among male and female in each group was 1644.15 ± 421 gm and 1570.25 ± 402 gm. Travers CP, et al. found the mean birth weight of 933 ± 328 gram and the average weight at the time of entry in study was 126833 ± 3 gm. In a study conducted by Yllescas, et al. the mean weight in nasal prongs and oxygen hood group was 1195 ± 517 gm and 1095 ± 319 gram respectively.
In our study the overall episodes of desaturation were total 124 (60.48%) and 74 (36.09%) in nasal prongs and oxygen hood. A similar study conducted by Travers CP, et al. found similar results, 130 ± 64 in nasal prongs group and 117 ± 77 episodes in oxygen environment (P value 0.002). The overall serious episodes of desaturation SpO2<85% were more in nasal prongs. In a study conducted by Travers CP, et al. found total 47 ± 47 episodes of severe desaturation in 24 hours with oxygen environment (hood) and 48 ± 38 in nasal prongs and results were similar to our study. Some of the multicentre controlled trials have shown that automatic control mode is superior to routine manual mode in prevention of oxygen fluctuation however; in our study the mode was manual.
The early and late apneic episodes were less with nasal prongs 27 (41.53%) as compared oxygen hood 38 (56.46%) however, the apneic episodes in both groups were not statistically significant (p value>0.05). Nasal prongs are better than hood in prevention of apneic episodes. The reason being the nasal prongs are put in nasal cavity directly and helps in splinting the airways and may generate some PEEP also. Other reason may be it increases the fractional residual capacity and decreases the work of breathing. The results of different study may vary as some studies have used flow rate of 2 L/minute in nasal prongs and 3-8 L/minute in hood however, we used flow rate of at 1 litre not 2.5 litre in nasal prongs. The flow rate and calibre of the canula size may affect the results of any study. In various trials, nasal prongs have been found to be more successful in preventing desaturation and CPAP failure, although they are not without risk of nasal injury.
In a large scale study conducted by Parmar J, et al. in Madhya Pradesh on rationalizing oxygen use, it was found that nasal prongs are convenient, well tolerated, cost effective and decrease oxygen consumption with minimal risk of nasal injuries. They are more cost effective and decrease the consumption of oxygen especially in developing countries however; we have not studied cost and oxygen consumption in our index study.
In a similar study by Yllescas, et al. Nasal prongs were found to be more effective as compared to oxygen hood in 84.8% versus 58.8% respectively however, no clinical differences were found between numbers of apneic episodes, desaturation. In our study the success rate with nasal prongs and oxygen hood was 77.27% and 54.54% respectively. Hensey CC, et al. showed that the treatment failure was more with air and sham as compared to oxygen. In another study by Woodhead D, et al. compared vapotherm with nasal canulla showed that the babies in vapotherm group performed better as compared to nasal cannula. One more study conducted by Di Fiore JM, et al. on 71 pre-term infants showed that hypoxic events increased with the increase in post-natal age and were associated with more chances of developing severe type of retinopathy requiring aggressive treatment, that is why it’s necessary to study the severity and duration of the hypoxic events.
The incidence of desaturation were more in first 12 hours with oxygen hood but not statistically significant. Study by Hensey, et al. showed that 94% of treatment failure was due to desaturation.
Why results are different with two devices?: The reason being the oxygen concentration varies with each breath when baby is breathing with open mouth, there is some leakage and it also depends upon the tidal volume and the inspiratory time. While the oxygen concentration is maintained uniformly inside the close lid hood. The factors affecting oxygenation includes are: Size of oxygen hood and of lid closure, the proper method of application, FiO2 and rate of flow of oxygen. Oxygen hood tries to maintain the set concentration of oxygen environment (FIO 21%-80%) but are not servo controlled. The other reason being that our mode is manual not servo controlled and different flow rates.
Conclusion
Desaturation was more commonly seen with the nasal prongs group as compared to hood group. The early and late apneic episodes were less with nasal prongs. Nasal prongs are better in terms of success. The most common cause of restart of CPAP was non-maintenance of oxygen saturation. Further such large scale studies are needed.
Study Implication
The babies who require some positive end expiratory pressure or suffering from more respiratory pathology should be put on nasal prongs, as they are more effective in prevention of apneic episodes and deliver some PEEP also. The disease where the saturation is the issue, baby should be put on oxygen hood as it provides more concentration and uniform environment resulting in lower desaturation episodes. We can cross over the two devices so that desaturation episodes and failure are balanced. When prolonged oxygen is required, then air alone or air oxygen mixture should be used by blender and FiO2 must be monitored to prevent severe hypoxic events.