Current Pediatric Research
International Journal of Pediatrics
Thoracoscopic clipping of open ductus arteriosus in premature infants: Progress in neonatal surgery.
Kemelbekov Kanatzhan1,4*, Nuskabayeva Gulnaz4, Datkayeva Gulmira1, Daniyarova Anara2, Dossybayev Murat2, Anambayeva Aigul3, Kuandykov Yerlan4, Bektenova Gulmira1, Makhatova Venera4,5, Rustemova Sandugash4, Babayeva Kumissay4, Tasbulatov Nurgeldi4
1 Department of Pediatrics, South Kazakhstan Medical Academy, Shymkent, Kazakhstan
2 Department of Pediatrics, Al-Farabi Kazakh National University, Almaty, Kazakhstan
3 Department of Pediatrics, S. Asfendiyarov Kazakh national medical University, Almaty, Kazakhstan
4 Department of Pediatrics, Khoja Ahmet Yassawi International Kazakh-Turkish University, Turkistan, Kazakhstan
5 Department of Pediatrics, Center for Continuous Professional Development Kazakhstan, Shymkent, Kazakhstan
- Corresponding Author:
- Kemelbekov Kanatzhan
Department of Pediatrics
South Kazakhstan Medical Academy
Kazakhstan
160000
Shymkent
Al-Farabi-1 square
Kazakhstan
Tel: +77085334300
E-mail: kanat-270184@mail.ru
Accepted date: April 6th, 2021
Currently, the closure cap used: open surgery, endovascular occlusion and thoracoscopic clipping of OAD. A special group of children are immature, premature children who are on artificial ventilation associated with persistent fetal circulation. The study analyzed the medical history of 97 premature newborns with this heart defect, which were in the "Regional perinatal center" of Zhambyl region in the period 2015-2019. On the basis of complex clinical and instrumental studies, the newborns were divided into groups according to gestational age, weight and dependence on the features of the open arterial duct. The results of surgical treatment were analyzed, identified risk factors and possible complications.
Keywords
Patent ductus arteriosus, Premature infants, Surgical treatment.
Introduction
Open Arterial Duct (OAD) is one of the most common defects. The incidence of OAD is inversely proportional to gestational age (GW) and birth weight (MT) and is 10-18% of all CHD. A long-functioning arterial duct in premature infants is usually a sign of morpho-functional immaturity of the cardiovascular system [1-5]. The smaller the gestational age of the newborn, the more often he finds OAD. In newborns weighing less than 2000 gr., OAD is detected in about 40%, and in children whose gestational age is 28-30 weeks-in about 80% of cases [6-9]. According to Fanaroff, the frequency of hemo dynamically significant functioning arterial duct (GFAP) in infants with very low body weight is 1251-1500 Gy it ranges from 13% to 49% in newborns weighing 501-750 gr [10].
Despite the information available in the literature on this issue to date, there is no consensus on the methods of treatment with OAD of premature infants. According to Ohlsson A and Walia R, the optimal timing for surgery for OAD ligation in premature infants remains uncertain [11-15].
The most proven method of treatment of OAD is surgical, originating in the first half of the XX century, when the first successful operation was performed, consisting in the ligation of OAD through left-sided thoracotomy. In the future, various modifications of the operation were proposed (crossing of the OAD, imposition of several ligatures, clipping of the OAD), which allowed to reduce the operational mortality (from 2%, according to R. E. Gross, 1952) and complications associated with the operation (bleeding when the duct wall is damaged, hematoma formation, recanalization of the OAD) [16-19,5].
However, thoracotomy itself is a traumatic procedure. The dissection of a large array of tissues of the chest wall causes a violation of respiratory function and pain in the early postoperative period. In addition, the long-term results of thoracotomy deserve a negative assessment. To date, there are a significant number of observations indicating the development of musculoskeletal disorders in patients who underwent thoracotomy in childhood (25%-33%) [5,11,20-22]. Its most frequent consequences are high standing of the shoulder or shoulder blade, dysfunction of the upper limb, deformation of the chest wall, scoliosis [23-25], lagging breast growth in girls, deterioration of the function of the lung on the side of the operation. Thoracotomy can also cause chronic chest pain. In addition, even a wide thoracotomy is not always able to provide the required quality of surgical access. This complicates the surgeon's manipulations and increases the risk of complications where perfect visualization and precision work with anatomical structures is required. Finally, cosmetic disorders in the form of rough postoperative scars themselves in some cases require additional surgical correction.
The emergence of minimally invasive technologies in surgery potentially makes it possible to avoid these problems, as evidenced by the experience of many authors [23-27]. In this regard, the search for new methods of treatment of OAD with minimal trauma and evaluation of their effectiveness becomes urgent.
One such technique is endovascular OAD occlusion, but this method has a number of limitations. To date, the most significant of them is considered to be the patient's body weight less than 5 kg with the size of the OAD more than 7 mm [28-30]. Cases of successful embolization in young children weighing less than 2.5 kg are isolated. The use of this technique involves a thorough study of the shape of the ductus arteriosus with measurement of its size at the preoperative stage in order to select the desired occluder. In addition, implantation of any occluder is accompanied by the risk of systemic and pulmonary embolism, hemolysis, and aneurysm formation [31-34]. Observations of recurrent laryngeal nerve paralysis after catheter OAD occlusion. The disadvantages of the method also include complications developing during vascular puncture, and radiation load on the patient. The efficiency of the method, according to different authors, is 88.0-95.0% [35-38].
Material and Methods
For the period from 1 January 2015 to 31 December 2019 in the Zhambyl Regional perinatal center and NCCT (Scientificclinical center of cardiology and transplantation) was performed in 97 operations clipping of PDA in patients body weight which at the time of operation was less than 2500 g. All these patients underwent comprehensive examination: clinical history, electrocardiography, radiography of the chest, echocardiography, and analysis of gas composition and acidbase status of blood. Depending on gestational age, weight and severity of the condition were divided into 2 groups. Newborns of the first group had gestational age, weight and height at birth less than in children of the second group.
Excluded from the study were: patients with OAD aneurysm; patients who were recorded in the operating logs, but whose medical records could not be raised (n=8). Patients who underwent OAD ligation through classical thoracotomy (n=3, medical records of two patients from this group could not be found in the archive) were included in the comparison group with patients who underwent thoracoscopic clipping of OAD.
Theory/Calculation
Treatment of OAD in premature newborns with low and extremely low body weight, which are in a serious condition and often have combined malformations, in particular, due to the small size of the chest, creating difficulties in accessing OAD, presents particular difficulties.
The relevance of this work is determined by the need to study the effectiveness of modern minimally invasive methods of treatment of OAD in children of different ages in different States.
The aim of the study was to determine the results of conservative therapy and surgical treatment with OAD in premature infants.
Results and Discussion
For further analysis on a random sample basis with a confidence level of 95% and confidence interval ± 5% were selected 92 patients who underwent clipping of PDA via a mini-thoracotomy with upplevelsen access (group I) and 69 patients who underwent thoracoscopic kierowanie RFP (group II). On the basis of complex clinical and instrumental studies, the newborns were divided into groups according to gestational age, weight and dependence on the features of the open arterial duct. The characteristics of the groups are presented in Table 1.
| Indicators | I group | II group | The difference of confidence (p = 0.05) according Mann-Whitney U-test criteria |
|---|---|---|---|
| Number of premature newborns | 72 | 25 | |
| Gestation period, weeks (M ± SD) | 28.8 ± 1.2 | 30.1 ± 272 | 0.003 |
| Birth weight, kg (M ± SD) | 1.3 ± 0.42 | 2.1 ± 0.4 | 0.037 |
| The average sequence pregnancy of the mother | 4 | 3 | |
| The diameter of the cap (at the Echo), mm | 2.6 ± 0.45 | 1.84 ± 0.64 | 0.042 |
| Circulatory insufficiency (NC) IIA-IIB degree, number of newborns (N. A. Belokon,1987.) | 31 | 4 | |
| Respiratory failure (DN) III degree, number of newborns (A.N.Anokhin, 1974) | 72 | 0 | |
| The endotracheal alveofact, the number of births | 41 | 3 | |
| The duration of mechanical ventilation, hours (M ± SD) | 279 ± 74.45 | 178 ± 77.53 | 0.008 |
| Comorbidity, Respiratory distress syndrome and Bronchopulmonary dysplasia, number of newborns | 70 | 12 | |
| Comorbidity, intraventricular hemorrhage II-III degree, the number of births | 64 | 11 | |
| Intrauterine infection and other infection | 13 | 1 | |
| Mortality (%) | 14 (19%) | 3 (12 %) | |
Table 1. Characteristics and risk factors of groups of premature newborns diagnosed with OAD.
The choice of treatment was determined by the severity of the patient's condition and his body weight (Table 2).
| Characteristic | I group | II group |
|---|---|---|
| Operative access | mini-thoracotomy | Thoracoscopy |
| Status | Heavy extremely difficult | Satisfactory Moderate |
| Body weight | any (including, very low and extremely low) | more than 2 kg |
| Number of operations (=Number of patients) | 72 | 25 |
Table 2. The choice of surgical intervention method depending on the severity of the patient's condition and body weight.
Characteristics of patients present in the first group. The first group included 72 children with OAD. Of these, 37 were boys and 35 were girls (Table 3).
| Sex | Number | % |
|---|---|---|
| Boys | 37 | 51.1 |
| Girls | 35 | 48.9 |
| Total | 72 | 100 |
Table 3. Distribution of group I patients by sex.
The median gestational age (IU) was 28.8 weeks (Q1-Q3:27.6-30.0 weeks). The median birth weight was 1300.0 gr (Q1-Q3:880.0-1720.0 g) (Table 4). Minimum body weight at birth is 620 gm.
| Parameter | Me | Q1-Q3 |
|---|---|---|
| Gestational age, week | 28.8 | 27.6-30.0 |
| Birth weight, gram | 1300 | 880.0-1720.0 |
Table 4. Distribution of group I patients by gestation period and birth weight.
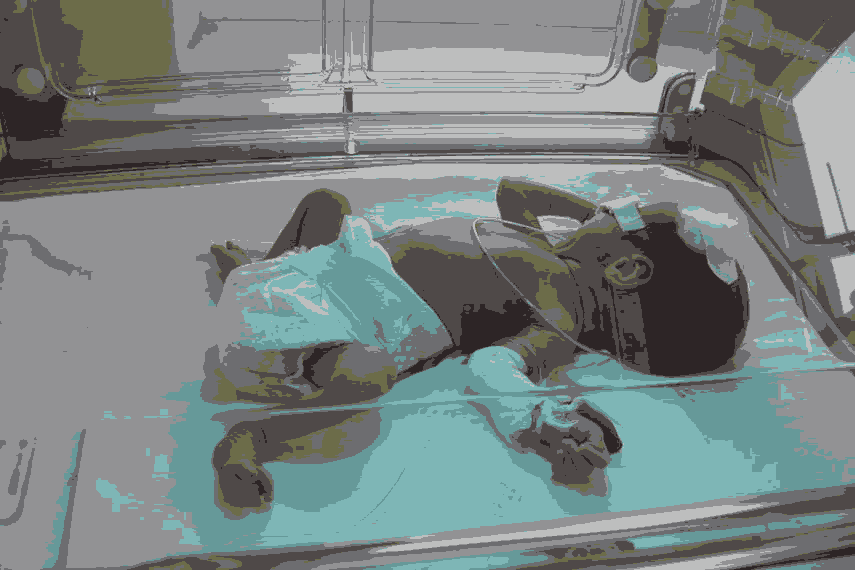
The 1st group (72 children) included premature infants, where the average gestational age at birth is 28.8 ± 1.2 weeks; the average weight is 1.3 ± 0.42 kg. The Above patients needed surgery for urgent indications. Indications for surgical intervention in preterm infants on mechanical ventilation was dependence on a ventilator, severe circulatory failure IIB-III degree of respiratory failure, the lack of effect from medical treatment, the instrumental confirmation of the importance of the cap for an ECHO -the presence of left-right discharge of blood through the PDA, volume overloading of the left cavities of the heart. Comorbidity-RDS in all newborns that required in 11(55%) cases of application of alveofact and 16(85.7%) intraventricular hemorrhage (IVH) II-III degree (Figure 1).
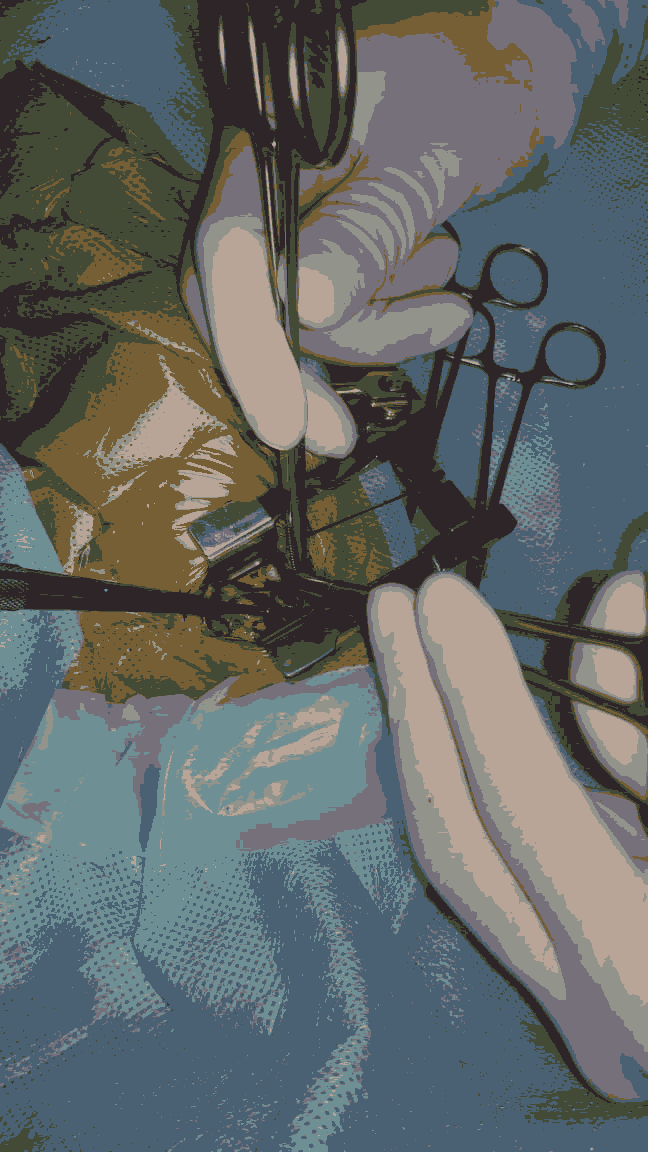
In the 1st group (open surgery) included 72 patients, which overlay the clips on the duct is made through the side of Tran’s axillary muscle-Clare Galway thoracotomy. Open operations were performed using a lateral incision of the chest about 1.5 cm long, which was performed in the axillary fossa, where there are no muscle arrays. The parietal pleura were dissected along the aorta from the site of the subclavian artery to the level of the thoracic aorta. Then allocate the cap. Particular attention was paid to the prevention of damage to the recurrent and vagus nerves.
Depending on the diameter of the OAD imposed 1 or 2 titanium clips of different sizes. When the diameter of the ductus arteriosus is 3 mm overlap clips medium size (Medium), vessel diameter greater than 3 mm closed clip big size (Medium-Large). The efficacy of the occlusion was controlled by an esophageal stethoscope placed in the esophagus before surgery. The air from the pleural cavity was evacuated with a vacuum aspirator. Drainage of the pleural cavity was not performed.
Characteristics of patients present in the second group: Patients of this group are children in stable (satisfactory or moderate severity) condition. In most cases, the detection of OAD in them was accidental during routine examinations and no symptoms of the disease, except for non-severe systolic noise, determined by auscultation, were noted.
In 4 children (5.8%) marked hemodynamic manifestations of OAD. In the preoperative period, they received complex treatment aimed at eliminating heart failure (diuretics, cardiac glycosides, ACE inhibitors).
The 2nd group (25 patients) premature infants, the average gestational age at birth were 30.1 ± 2.72 weeks, the average weight of 2.1 ± 0.4 kg. Usually they were on independent breath, the clinic NC various degrees, without significant impairment of respiratory function. Group 2 (thoracoscopic surgery) consisted of 25 patients. Thoracoscopic procedures required special video endoscopic equipment, so we performed them exclusively in the children's hospital. In children weighing less than 2500 g used a 30° telescope with a diameter of 3.9 mm (Karl Storz GmbH, Tuetlingen, Germany), 3 mm instruments for dissection of tissues, 5 mm or 10 mm endoscopic clipprinter. One-lung artificial ventilation was used.
In the distribution of patients according to sex, there was a slight predominance of female over male (girls 56%, boys 44%).
The minimum body weight was 2 kg in the patient 11 days of life, the maximum-15 kg in the patient 3 years 7 months. Median body weight 8.5 kg (Q1-Q3: 2.0-15.0 kg); median age 1 g 8 months (Q1-Q3: 11 days 3 years 7 months) (Table 5).
| Parameter | Me | Q1-Q3 |
|---|---|---|
| Age | 1 year 8 months | 11 day-3 years 7 months |
| Body weight | 8.5 kg | 2.0-15.0 kg |
Table 5. Distribution of group II patients by age and body weight at the time of surgery.
Observation of patients of both groups consisted in performing chest x-ray examination 1 hr after surgery to control possible accumulation of air in the hemitorax, as well as echocardiography the next day after surgery. Disconnection from the ventilator became possible after the restoration of adequate self-breathing. After stabilization of respiratory and hemodynamic status, patients were transferred to the nursing Department of premature babies. Control of postoperative complications was performed during the patients' stay in the hospital and during repeated visits 1, 3, 6 and 12 months after discharge.
Clipping time of OAD via mini-thoracotomy access was 20.2 ± 5.2 minutes (minimum value: 15 minutes, maximum value: 25.4 minutes). The size and shape of the ductus arteriosus ranged from 1 mm, 84 mm to 2.6 mm (inner diameter of the cap according to EchoCG), from 2 mm to 5 mm wide (intra - operating dimensions), cylindrical, apollobravo forms, from very short to 8 mm in length. 95.12% of group I patients managed to achieve complete cessation of blood flow through OAD. In two children with a duct diameter of 2 and 3 mm in the postoperative period, there was a residual discharge of blood by OAD with a diameter of 1.1 and 2.3 mm, respectively. However, hemodynamic parameters in these patients stabilized after surgery, and residual shunt was not hemodynamically significant for these children (Figure 2).
Intraoperative mortality and mortality associated with surgical complications were not observed in our series of observations. Hospital mortality in the postoperative period was 5.43% and was associated not with surgery, but with the phenomena of severe morphofunctional immaturity, severe malformations, uncontrolled infectious complications that aggravated the manifestations of heart and respiratory failure (Table 6).
| Parameter | Number of patients, n=72 | % |
|---|---|---|
| Intraoperative transfusion of blood components: | ||
| Erythrocyte mass | 2 | 2.3 |
| Fresh frozen plasma | 55 | 84.5 |
| Intraoperative bleeding | 2 | 2.1 |
| Installing a chest drainage | 2 | 2.1 |
Table 6. Intraoperative data in mini-thoracotomy.
The results of statistical analysis (Wilconson criterion was used for evaluation) showed a statistically significant decrease in hemodynamic parameters after clipping OAD (p<0.05) (Table 7).
| Indicator/symptom | Before surgery Me (Q1-Q3) | After surgery (1-3 days) Me (Q1- Q3) |
P |
|---|---|---|---|
| Open arterial duct diameter, mm | 2.6 ± 0.45 (2.15-3.05) | <0.05 | <0.001* |
| Blood flow through the open ductus arteriosus | Eat (n=72; 100%) | No (n=69; 95.4%) Residual (n=5; 4, 0.6%) |
|
| Direction the blood flow through the PDA | ??-P? 1 | Ao/PA 2 (n=69; 95, 0.4%) Ao-PA (n=3; 4, 0.6%) |
|
| Character of blood flow in LP? 3 | Changed (with antegrade diastolic flow) | Not changed (trunk) | |
| The diameter of the OAD/m 4, mm/kg | 2.6 (2.15-3.05) | <0.01 | <0.001* |
| LP/?? 5 | 1.37 (1.67-1.92) | 1.26 (1.7-1.73) | <0.001* |
| EDS/?? 6 | 2.15 (1.72-2.28) | 1.79 (1.16-1.92) | 0.001* |
| *: Differences in indicators are statistically significant (p<0.05) | |||
| 1: Ao-PA-direction of OAD blood flow from the aorta to the pulmonary artery | |||
| 2: Ao/PA-blood flow in the aorta and pulmonary artery is divided | |||
| 3: Left Pulmonary Artery | |||
| 4: m-baby's body weight at the time of the study | |||
| 5: LP/AO-ratio of anterior-posterior size of the left atrium to the base of the aorta | |||
| 6: EDS/Ao - the ratio of end-diastolic size of the left ventricle to the base of the aorta. | |||
Table 7: Changes in hemodynamic variables after closing the cap.
We in the work, at studying of various risk factors (characteristics of a somatic condition of the child) which, according to our supervision, in the greatest degree influenced survival of children.
As a result, a group of factors was formed, comparable with the aggravating signs studied in the literature. Each of them had a significant impact on mortality: the degree of prematurity and the presence of concomitant disease (p<0.05), early neonatal age-up to 7 days of life (p<0.05). The most important in this case had a combination of low weight to = 1000 g and prematurity (28-30 weeks) (p<0.001), IUI (p<0.001), ventilator before surgery (p <0.001), somatic diseases (RDS, pneumonia and FGM) (p<0.001). Our observations confirmed that in children without risk factors the outcomes of surgical treatment are the most favorable, regardless of the type of intervention. However, characterizing the severity of the somatic condition of the patient by the number of factors regardless of their combination, each addition of one factor worsens the outcomes of treatment (p<0.001). At the same time, a combination of three risk factors can be considered a “critical” level. On the basis of the data obtained, specific dynamic steps in the treatment of children depending on risk factors were formulated, which influenced both the increase in the number of operated newborns over the years and the decrease in total surgical mortality in group I (up to 11.7%) than in group II (15%).
The results showed that long-term functioning of the OAD directly affects the duration of ventilation, and, as a consequence, leads to the development of BPD (12.7% in the General group) and high mortality. With the ineffectiveness of drug therapy, such children need to perform immediate surgery, despite the severity of the initial state - prematurity, low weight, - as well as the complexity associated with the transportation of such patients in a specialized cardiac hospital. Thus, a distinctive feature of cardiac surgery in the neonatal period is the "inability to wait" until the child gains weight, is cured of VUI, ventilator-associated pneumonia, is stabilized by heart failure after prolonged transportation and so on. The expansion of indications for surgery with a confident positive outcome is possible with an increase in the quality of the surgery itself, anesthetic benefits and nursing, including the management of children in the early postoperative period.
Conclusion
Advanced technique of thoracoscopic clipping of PDA allows its closure in children of any age and with any body weight, including preterm low birth-weight babies’ posterolateral access. Technology is clipping the cap via a mini-thoracotomy with upplevelsen access allows to achieve the complete cessation of blood shunting at the PDA in the first day after surgery in 95.4% of children, and termination of clinically significant relief of blood-100%; transfer from ventilator to independent breathing - more than 68% of children. Thoracoscopic clipping of OAD in children allows in 100% of cases to stop the blood flow through the functioning OAD, regardless of its shape and size. Timely surgical elimination of hemodynamically significant PDA in preterm infants decreases the duration of stay on a ventilator. Surgical intervention in a premature newborn with OAD is accompanied by a small number of complications and low postoperative mortality.
References
- Albayrak G, Aykut K, Karacelik M, et al. Bedside surgery to treat patent ductus arteriosus in low-birth- weight premature infants. Open Journal of Cardiovascular Surgery. 2016;7:1-4.
- Backes CH, Rivera BK, Bridge JA, et al. Percutaneous Patent Ductus Arteriosus (PDA) closure during infan: A meta-analysis. Pediatrics. 2017;139(2):e20162927.
- Benitz WE. Patent ductus arteriosus: To treat or not to treat?. Arch Dis Child Fetal Neonatal Ed. 2012;97(2):F80-2.
- Benson LN. The Arterial Duct: Its persistence and its patency. Paediatric Cardiology. Ed. by Philadelphia: Churchill Livingstone. 2019;875-93.
- Deshpande P, Baczynski M, McNamara PJ, et al. Patent ductus arteriosus: The physiology of transition. Semin Fetal Neonatal Med. 2018;23(4):225-31.
- Demirturk O, Güvener M, Coskun I, et al. Results from extrapleural clipping of a patent ductus arteriosus in seriously ill preterm infants. Pediatr Cardiol. 2017;8(32):1164-7.
- Fadel BM, Mohty D, Husain A, et al. The various hemodynamic profiles of the patent ductus arteriosus in adults. Echocardiography. 2015;7(2):1172-8.
- Garcia AV, Lukish J. Minimally invasive patent ductus arteriosus ligation. Clin Perinatol. 2017;44(4):763-71.
- García-Tirado J, Rieger-Reyes C. Suture Techniques of the intercostal space in thoracotomy and their relationship with post-thoracotomy pain: A systematic review. Archivos de Bronconeumología (English Edition). 2019;48(1):22-8.
- Bose CL, Laughon MM. Patent ductus arteriosus: lack of evidence for common. Arch Dis Child Fetal Neonatal Ed. 2017;92(6):498-502.
- Brunner B, Hoeck M, Schermer E, et al. Patent ductus arteriosus, low platelets, cyclooxygenase inhibitors, and intraventricular hemorrhage in very low birth weight preterm infants. J Pediatr. 2013;163(1):23-8.
- Gray DT, Fyler DC, Walker AM, et al. Clinical outcomes and costs of transcatheter as compared with surgi- cal closure of patent ductus arteriosus. N Engl J Med. 2017;329(21):1517-23.
- Herrman K, Bose C, Lewis K, et al. Spontaneous closure of the patent ductus arteriosus in very low birth weight infants following discharge from the neonatal unit. Arch Dis Child Fetal Neonatal Ed. 2019;1(94):48-50.
- Heuchan AM, Clyman RI. Managing the patent ductus arteriosus: current treatment options. Arch Dis Child Fetal Neonatal Ed. 2014;99(5):F431-6.
- Huanga X, Wangb F, Wangb K. Paracetamol versus ibuprofen for the treatment of patent ductus arteri- osus in preterm neonates: a meta-analysis of randomized controlled trials (Review). J Matern Fetal Neonatal Med. 2017;31(16):2216-22.
- Inaba H, Higuchi Ka, Koseni K, et al. Surgical closure of adult patent ductus arteriosus using a pursestring suture. Asian Cardiovasc Thorac Ann. 2018;16(1):59-61.
- Keating P, Verhagen E, van Hoften J, et al. Effect of indomethacin infused over 30 minutes on cerebral fractional tissue oxygen extraction in preterm newborns with a patent ductus arteriosus. Neonatology. 2016;98(3):232-7.
- King H, Mandelbaum I. Extrapleural approach for patent ductus arteriosus. Surgery. 2016;51:277-9.
- Koch Jm, Hensley G, Roy L, et al . Prevalence of spontaneous closure of the ductus arteriosus in neonates at a birth weight of 1000 grams or less. Pediatrics. 2016;4(117):1113-21.
- Laborde F, Noirhomme P, Karam J, et al. A new video-assisted thoracoscopic surgical technique for interruption of patient ductus arteriosus in infants and children. J Thorac Cardiovasc Surg. 1993;2(105):278-80.
- Laurin S, Sandström S, Ivancev K, et al. ductus arteriosus aneurysm imaging using modern diagnostic meth-ods. Acta Radiologica. 2015;33(4):285-91.
- Lee GY, Sohn YB, Kim MJ, et al. Outcome following surgical closure of patent ductus arteriosus in very low birth weight infants in neonatal intensive care unit. Yonsei Med J. 2018;49(2):265-69.
- Leon-Wyss J, Vida VL, Veras O, et al. Modified extrapleural ligation of patent ductus arteriosus: a conven- ient surgical approach in a developing country. Ann Thorac Surg. 2015;2(79):632-5.
- Levin M, McCurnin D, Seidner SR et al. Seidner postnatal constriction, ATP depletion, and cell death in the ma- ture and immature ductus arteriosus. AJP-Regul Integr Comp Physiol. 2016;290:R359-64.
- Liang CD, Ko SF, Huang SC, et al. Vocal cord paralysis after transcatheter coil embolization of patent ductus arteriosus. Am Heart J. 2013;2(146):367-71.
- Liem NT, Tuan TM, Linh NV. A safe technique of thoracoscopic clipping of patent ductus arteriosus in children. J Laparoendosc Adv Surg Tech A. 2017;4(22):422-4.
- Lin CT, Liu WH, Cheng BC, et al. Surgical closure of patent ductus arteriosus in preterm infants at neonatal intensive care unit. Acta Paediatr Taiwan. 2018;5(44):287-91.
- Little DC, Pratt TC, Blalock SE, et al. Patent ductus arteriosus in micropreemies and full-term infants: the relative merits of surgical ligation versus indomethacin treatment. J Pediatr Surg. 2017;38(3):492-6.
- Malone PS, Cooper SG, Elliott M, et al. Aneurysm of the ductus arteriosus. Arch Dis Child. 2018;64(10):1386-8.
- Mandhan PL, Samarakkody U, Brown S, et al. Comparison of suture ligation and clip application for the treatment of patent ductus arteriosus in preterm neonates. J Thorac Cardiovasc Surg. 2016;3(132):672-4.
- Memisoglu A, Alp Ünkar Z, Cetiner N, et al. Ductal closure with intravenous paracetamol: a new approach to patent ductus arteriosus treatment. J Matern Fetal Neonatal Med. 2016;29(6):987-90.
- Murray L, Hendren WH, Mayer JE, et al. A thrill of extreme magnety: Robert E, Gross and the beginnings of cardiac surgery. J Pediatr Surg. 2018;8(48):1822-5.
- Naulaers G, Devriendt K, Moerman P, et al. Aneurysm of the ductus arteriosus in a neonate with 13q-deletion. Am J Perinatol. 2017;1(18):11-14.
- Niinikoski H, Alanen M, Parvinen T, et al. Surgical closure of patent ductus arteriosus in very-low-birth-weight infants. Pediatr Surg Int. 2016;17(5-6):338-41.
- Ohlsson A, Walia R, Shah SS. Ibuprofen for the treatment of patent ductus arteriosus in preterm and/or low birth weight infants (Review). The Cochrane Library. 2019;4:16-27.
- Oncel MY, Erdeve O. Oral medications regarding their safety and efficacy in the manage- ment of patent ductus arteriosus. World J Clin Pediatr. 2016;5(1):75-81.
- Porstmann W, Wierny L, Warnke H. Der verschluß des ductus arteriosus persistens ohne thorakotomie. The Thoracic and Cardiovascular Surgeon. 2016;15(02):199-203.
- Riggle M, Rice-Townsend SE, Waldhausen JHT. Thoracoscopic division of vascular rings. J Pediatr Surg. 2017;52(7):1113-7.