Current Pediatric Research
International Journal of Pediatrics
Surgical treatment?s possibilities of late adhesive intestinal obstruction in children.
BodnarOleh1*, Konoplitskyi Viktor2, KhashchukVasyl3, ProniaievDmytro4, Randiuk Roman5
1Department of pediatric surgery and otorhinolaryngology, Bukovinian State Medical University (BSMU), Chernivtsi, Ukraine
2Department of pediatric surgery, National Pirogov Memorial Medical University, Vinnytsya, Ukraine
3Department of pediatric surgery and otorhinolaryngology, Bukovinian State Medical University (BSMU), Chernivtsi, Ukraine
4Department of anatomy, clinical anatomy and operative surgery, Bukovinian State Medical University (BSMU), Chernivtsi, Ukraine
5Department of pediatric surgery and otorhinolaryngology, Bukovinian State Medical University (BSMU), Chernivtsi, Ukraine.
- Corresponding Author:
- Bodnar Oleh
Department of pediatric surgery and otorhinolaryngology
Bukovinian State Medical University (BSMU)
Chernivts
Ukraine
Tel: +38(050)6713283
E-mail: oleg1974rol@gmail.com
Accepted date: May 6, 2021
Citation: Farvardin M, Johari MK, Nami M, et al. Annular choroidal detachment one year after argus-II retinal prosthes is implantation. Ophthalmol Case Rep. 2020;4(1):23-25.
Objectives: To study the adhesions prevalence in the abdominal cavity and to determine the possibilities of surgical treatment of Late Adhesive Intestinal Obstruction (LAIO) in children.
Materials and Methods: 73 children were operated on for LAIO. 35 children were in a comparison group (comprehensive treatment by traditional methods) and 38 children were in the main group. In the main group was used an anti-adhesive solution which containing sodium hyaluronate and decamethoxin to prevent recurrence of Adhesive Intestinal Obstruction (AIO). The following surgical interventions were performed: Adhesiolysis, adhesiolysis and resection of the small intestine, adhesiolysis and making of the ileostomy, elimination of the cause without total adhesiolysis, elimination of the cause without total adhesiolysis and with resection of the small intestine, elimination of the cause without total adhesiolysis and with making of ileostomy. The Adhesion Process (AP) in the abdominal cavity was evaluated by the type of adhesions and their projection on the anterior abdominal wall.
Results: The most common causes of LAIO were adhesive conglomerates (32.88%), moorings (23.28%) and visceral-visceral adhesions (21.92%) in lesser extent visceral-parietal and omentalvisceral adhesions, accordingly 10.96% and 10.96%. In main group recurrent AIO was seen in 3 of 38 children (7.89%) and resolved conservatively. In comparison group recurrent AIO occurred in 7 of 35 children (20%). In comparison group, 4 of 7 children required relaparotomy. The method of cause eliminating was used at AIO without total adhesiolysis using sodium hyaluronate for the operated children. When children were observed between 1 and 7 years, recurrence of AIO was in 1 patient who resolved conservatively.
Conclusion: Mesothelium damaging leads to the emergence of the primary AP of the abdominal cavity with spreading to the surrounding structures and projection on the areas of the anterior abdominal wall. In operations for LAIO in children, it is advisable to use the operation of the cause eliminating (separation or resection of the conglomerates, cutting of the mooring) without total adhesiolysis in combination with intraoperative use of sodium hyaluronate solution with decamethoxine.
Keywords
Late Adhesion Intestinal Obstruction (LAIO), Children.
Introduction
Surgery for AIO in children is up to 4.2% of the total number of abdominal operations. 30% of patients with AIO are readmitted to surgical hospitals within 4 years. Open surgery is the best way to treat AIO in the absence of conservative effect of treatment in case of strangulation [1].
The selection of patients with AIO for laparoscopy remains a controversial issue. It is believed that the factors for successful laparoscopy are: the number of previous laparotomies is less than 2, the absence of midline laparotomy, appendectomy is the primary disease, presence of single “mooring”, the onset of AIO less than 24 hours, absence of symptoms of peritonitis. The operation consists of visualization of the caecum and proximal following with the intersection of the cause of AIO in the area of the transition zone, control of the restoration of the passage of the chyme. Adhesion conglomerates, dense and intense of AP are an indicator for the transition to laparotomy [2].
In 20% of open laparotomy is advisable due to hyperplastic AP and the possibility of iatrogenic damage to the abdominal cavity organs [3]. Contributing factors to the AP are the number of laparotomies and the duration of peritonitis. The incidence of requiring re-intervention after lower laparoscopic surgery AP is up to 2%, after colorectal surgery is up to 4% and 0.76% after appendectomy [4]. A variety of surgical techniques and barrier solutions are available to treat children with AIO [5-7].
Materials and Methods
A total of 245 patients with LAIO were examined for the period from 2005 to 2020 in age from 3 to 17 year-old. Conservative treatment was successful in 172 children, 73 children were operated on. For recurrent LAIO were hospitalized 21 children, 11 children underwent surgery (Table 1).
| Previous disease | Number of children | Number of operated children | The percentage of surgical operations according to the pathology, % |
|---|---|---|---|
| Catarrhal appendicitis | 7 | 2 | 28.57 |
| Destructive appendicitis | 35 | 6 | 17.14 |
| Destructive appendicitis+local peritonitis | 44 | 9 | 20.45 |
| Destructive appendicitis+diffuse/ generalized peritonitis | 48 | 15 | 31.25 |
| Injuries of Abdominal Cavity Organs (ACO) | 25 | 10 | 40 |
| Intestinal obstruction | 24 | 9 | 37.5 |
| Congenital diseases of ACO | 21 | 5 | 23.81 |
| Pathology of gynecology | 16 | 3 | 18.75 |
| Urological laparotomy operations | 2 | 1 | 50 |
| Recurrent LAIO | 21 | 11 | 52.38 |
| Kidney transplantation | 1 | 1 | 100 |
| Liver transplantation | 1 | 1 | 100 |
| Total | 245 | 73 | 29.8 |
Table 1: Children’s distribution by the occurrence of LAIO depending on the previous diseases.
Indications for laparotomy were: ineffectiveness of conservative therapy for 24 hours from its onset; deterioration of the patient's condition during conservative therapy for 12 hours; symptoms of peritonitis and strangulation (after 2 hours of preoperative preparation). Of the operated: 35 children were a comparison group (comprehensive treatment by traditional methods) and 38 children-the main group (Table 2).
| Surgical interventions | Main group | Comparison group |
|---|---|---|
| Adhesiolysis | 12 | 13 |
| Adhesiolysis and resection of the small intestine | 6 | 4 |
| Adhesiolysis with ileostomy | 1 | 1 |
| Elimination of the cause without total adhesiolysis | 12 | 13 |
| Elimination of the cause without total adhesiolysis and resection of the small intestine | 6 | 3 |
| Elimination of the cause without total adhesiolysis and ileostomy | 1 | 1 |
| Total | 38 | 35 |
Table 2: Distribution of children with LAIO, according to the performed surgical interventions (n=73).
In the main group of children in order to prevent recurrence of AIO used an anti-adhesive solution containing sodium hyaluronate and decamethoxine. The choice of relaparotomy site was an important stage of surgery.
Relaparotomy site
At AIO in the case of appendicitis, performed a median laparotomy, in the case of primary surgery for AIO performed a laparotomy incision with excision of the old postoperative scar, in the case of repeated operations for AIO, performed a laparotomy elsewhere (not on the old scar). This was done due to the hyperplasticity of the AP in secondary relaparotomy for AIO, the possibility of iatrogenic damage of the abdominal cavity structures and the involvement of abdominal organs in the adhesion with the parietal peritoneum of the scar.
Adhesiolysis
Adhesiolysis based on the principle of "from simple to complex". The loop of the small intestine was released from adhesions by dissecting the adhesions with a diatermocoagulator in the proximal and distal directions until complete release of intestinal loops. The condition of the intestinal loops was assessed, if necessary, resection was performed with the imposition of an ileo-ileoanastomosis “end to end”. Chyme was moved from the small intestine, starting from the ligament of Treitz to the large intestine through the ileocecal valve.
Ileostomy
The removal of the ileostomy was due to the signs of peritonitis, infiltrative-inflammatory changes of the distal ileum and the serious condition of children. The imposition of a primary anastomosis was unwarranted due to the high risk of postoperative complications. Resection of the terminal section was performed for 10 to 40 cm. The distal part of the ileum was 3 to 10 cm long. It was necessary to preserve the largest part of the distal part of the ileum and suture it to the parietal peritoneum of the lateral wall of the abdominal cavity.
An overlay of a single-stemmed (terminal) ileostomy was performed in the left iliac region. The ileostomy was performed by forming a peritoneal-muscular-aponeurotic layer with subsequent fixation of the intestinal wall to it. From the abdominal cavity, the mesentery of the stoma area was fixed in the avascular zone to the anterior-lateral wall of the abdomen to prevent evagination. Operations for intestinal continuity restoring began with the "stoma" stage of the surgery. Two enveloping stoma sections, using an electrocoagulator, dissected the skin, subcutaneous tissue.
The ileum was released from the aponeurotic muscle and peritoneum, freeing the mesenteric margin. A part of a sterile glove according to the diameter was placed on the stoma. This corresponded to the conditions of maintaining sterility during the surgery.
The next step was performing a right-side transrectal laparotomy. Isolation of the distal part of the blind part of the ileum, even with a significant development of the AP, was not difficult due to its fixation during the previous operation. The blind part of the ileum was taken on the suture holder, and the steel area was moved into the abdominal cavity.
When the distance of the distal part of the ileum from the ileocecal valve is more than 5 centimeters and the diameter of the blind end of the Iileum 1/2 and more proximal, ileoileoanastomosis was applied “end to end” using L-type serousmuscular and inverted through sutures (Figure 1).
When distance of the distal part of the ileum from the ileocecal valve is less than 5 centimeters and (or) the diameter of the blind end of the ileum less than 1/2 proximal performed terminal ileoileoanastomosis end to side with dissection of the distal part of the ileum along the antimesenterical edge according to the diameter of the proximal part.
The anastomosis was performed with nodular serousmuscular and inversion through sutures (Figure 2).
Elimination of the cause without total adhesiolysis. There are causes of LAIO: “moorings” or adhesive conglomerate. The cause was eliminated by dissection of adhesions, release of the conglomerate.
In case of intestinal necrosis, resection was performed, in case of impossibility of the adhesion conglomerate separation without significant damage to the structures, resection of the latter was performed. Intestinal patency was assessed without total adhesiolysis.
Features of barrier solution using (“Defensal”: Sodium Hyaluronate and Decamethoxine) in the main group of children. The antiadhesion solution was poured into the abdominal cavity in the amount of 250 ml for children under
10 years and 500 ml for children after 10 years. The peritoneum was sutured with a continuous suture (Vicril 3/0, Vicril 2/0), starting from the lower corner of the wound to the middle of the wound.
Next, similarly continuously sutured the peritoneum from the upper corner of the wound to the middle. Two nodal sutures were applied through the aponeurosis and peritoneum as holders. A male catheter ? 16 was inserted into the abdominal cavity between the sutures.
The upper part of the aponeurosis and the lower part to the sutures of the holders were continuously sutured. The catheter was connected to a container of sodium hyaluronate, and the catheter was moved clockwise in the abdominal cavity while lifting the sutures of the holders, introducing the hyaluronate solution (starting and ending in the right subhepatic space).
The sutures were tied. The subcutaneous tissue and skin were sutured. This method allows you to fill the barrier solution, adhering to antiseptics and preventing it from leaking out of the abdomen.
Adhesions are an obstacle to the functioning of the gastrointestinal tract only when they cause pain and obstruction. Therefore, during the intraoperative examination of the abdominal cavity, adhesions and AP were evaluated according to the following criteria: 1: Primary localization of AP; 2: Types of adhesions; 3: Distribution of AP. Primary localization of the AP.
Primary surgery leads to various types of adhesions, which in the future is the basis for the use of a particular method of treatment.
Primary localization means the place of primary occurrence of the AP, which is due to the place of damage to the memorial (intestinal necrosis and subsequent resection), the place of the reserve process and the installation of drainage (acute appendicitis, peritonitis, adnexitis), the location of blood in the abdomen.
The location of the primary localization of the AP, although it cancels the key role in its further spread and treatment.
Types of adhesions: "moorings" (connective tissue tape that extends from the visceral organ to the visceral organ, or from the visceral organ to the parietal peritoneum); visceralparietal (between the visceral organ and the parietal peritoneum); visceral-visceral; omental-visceral and adhesive conglomerates (contain all the above features).
Distribution of AP
The spread of the AP was understood as the extent of the spread of the AP from the place of primary localization to the abdominal cavity with the impact of the visceral organs, large omentum, anterior abdominal wall and dysfunction of the latter.
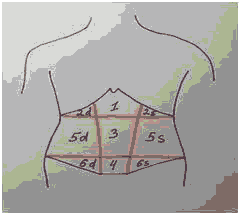
The well-known divisions of the abdominal wall into areas on which the structures of the abdominal cavity are projected: 1: Regioepigastrica propria, 2: Regiohypochondrica (dextra et sinistra (2d, 2s), 3: Regioumbilicalis, 4: Regiopubicum, 5: Regioabdominalis lateralis (dextra et sinistra (5d, 5s), 6: Regiounqinalis (dextra et sinistra (6d, 6s). The AP from its initial origin spread and projected on the areas of the anterior abdominal wall (Figure 3).
| Previous disease | Number of children | Types of adhesions and their number in the group | ||||
|---|---|---|---|---|---|---|
| “moorings” | Visceral- visceral adhesions | Visceral- parietal adhesions | Omental-visceral adhesions | Adhesive conglomerate | ||
| Catarrhal appendicitis | 2 | |||||
| Destructive appendicitis | 6 | 2 | 5 | 3 | 3 | - |
| Destructive appendicitis + local peritonitis | 9 | 2 | 8 | 7 | 6 | - |
| Destructive appendicitis +diffuse/ generalized peritonitis |
15 | 3 | 10 | 9 | 12 | 5 |
| Injuriesof ACO | 10 | 3 | 9 | 7 | 7 | 1 |
| Intestinal obstruction | 9 | 3 | 9 | 6 | 7 | 3 |
| Congenital diseasesof ACO | 5 | 1 | 5 | 4 | 4 | 1 |
| Pathology of gynecology | 3 | 1 | 3 | 2 | 2 | 1 |
| Urological laparoto my | 1 | - | 1 | 1 | 1 | - |
| operations | ||||||
| Recurrent LAIO | 1 | - | 1 | 1 | 1 | 1 |
| Kidney transplantation | 1 | - | 1 | 1 | 1 | 1 |
| Liver transplantation | 11 | 3 | 11 | 11 | 11 | 11 |
| Total | 73 | 19 | 65 | 52 | 57 | 23 |
Results and Discussion
When assessing the AP, according to the primary localization, in all cases it was detected at the site of surgery or at the site of mesothelial damage. Thus, in the case of kidney transplantation, which was preceded by peritoneal dialysis, the place of primary localization was considered the entire abdominal cavity, because the damage to the mesothelium was throughout the visceral and parietal peritoneum (Figure 1). In the case of catarrhal appendicitis, the place of primary localization of the AP was the right iliac region. It was important to assess the AP by type of adhesions depending on the previous operation, which allowed to determine the extent of surgery (Table 3).
To determine the tactics of surgical treatment, it was important to assess the cause of LAIO, because in many cases it makes sense to eliminate only the cause, not performing total
adhesiolysis, which if performed will lead to more hyperplastic adhesions in the abdomen (Table 4).
| Previous disease | Number of children | Types of adhesions | ||||
|---|---|---|---|---|---|---|
| “moorings” | Visceral- visceral adhesions | Visceral- parietal adhesions | Omental visceral adhesions | Adhesive conglomerate | ||
| Catarrhal appendicitis | 2 | |||||
| Destructive appendicitis | 6 | 2 | 1 | 1 | 2 | - |
| Destructive appendicitis+local peritonitis | 9 | 2 | 5 | 1 | 1 | - |
| Destructive appendicitis +diffuse/ generalized peritonitis |
15 | 3 | 3 | 2 | 2 | 5 |
| Injuries of ACO | 10 | 3 | 3 | 2 | 1 | 1 |
| Intestinal obstruction | 9 | 3 | 1 | 1 | 1 | 3 |
| Congenital diseases of ACO | 5 | 1 | 1 | 1 | 1 | 1 |
| Pathology of gynecology | 3 | 1 | 1 | - | - | 1 |
| Urological laparoto | 1 | - | 1 | - | - | - |
| my operations | ||||||
| Recurrent LAIO | 1 | - | - | - | - | 1 |
| Kidney transplantation | 1 | - | - | - | - | 1 |
| Liver transplantation | 11 | - | - | - | - | 11 |
| Total | 73 | 17 | 16 | 8 | 8 | 24 |
Table 4: Adhesions that have caused relaparotomy in children with LAIO.
Thus, the most common causes of LAIO were adhesive conglomerates (32.88%), moorings (23.28%) and visceralvisceral adhesions (21.92%) in lesser extent visceral-parietal and omental-visceral adhesions, accordingly 10.96% and 10.96%.
The most common hyperplastic AP was observed in the case of kidney transplantation, which was due to previous peritoneal dialysis in a child. The change in the normal anatomy of the ACO was in AIO in the case of liver transplantation. When separating the adhesions, it was necessary to know the course of the previous surgery. Diffuse peritonitis when using drainage techniques were subsequently accompanied by significant adhesions with deserosion and damage to the mesothelium during their separation.
It should be noted that when using drainage methods of local (42 children), diffuse (19 children) and generalized peritonitis laparotomy access (17 children) and abdominal lavage with ozonated NaCl 0.9% at concentration of 3-5 mg / l, the development of AIO was observed only in 1 child in the case of local peritonitis and 2 children after diffuse peritonitis, during 7 years of the postoperative period. The signs of LAIO at these children were bought up by conservative therapy. Significant hyperplastic AP was found in 11 children with recurrent AIO (Table 5).
| Pathology | Number of children | Projection on the anterior abdominal wall according to the ? |
|---|---|---|
| Catarrhal appendicitis | 2 | 6d+5d+3 |
| Destructive appendicitis | 6 | 6d+5d+3 |
| Destructive appendicitis | 9 | 6d+5d+3+4 |
| +local peritonitis | ||
| Destructive appendicitis | 15 | 6d+5d+3+4+5s+6s |
| +diffuse/generalized peritonitis | ||
| Injuries of ACO | 10 | 2d+1+2s+3+5d+5s ??? |
| 2d+1+3+5d ??? | ||
| 1+2s+3+5s+4+6 | ||
| Intestinal obstruction | 9 | 2d+1+2s+3+5d+5s ??? |
| 2d+1+3+5d ??? | ||
| 1+2s+3+5s+4+6 | ||
| Congenital diseases of ACO | 5 | 2d+1+2s+3+5d+5s ??? |
| 2d+1+3+5d ??? | ||
| 1+2s+3+5s+4+6 | ||
| Pathology of gynecology | 3 | 6d+4+6s ??? |
| Urological laparotomy operations | 6d+4+6s+5d+3+5s | |
| Recurrent LAIO | 1 | 5d+3+5s+6d+4+6s |
| Kidney transplantation | 1 | between 1 and 6 |
| Liver transplantation | 1 | between 1 and 6 |
| Liver transplantation | 11 | between 1 and 6 |
| Total | 73 |
Table 5: Significant hyperplastic AP was found in children with recurrent AIO.
The projection of AP on the anterior abdominal wall by areas should be used to select the method of surgical treatment of LAIO and select the location of trocars for laparoscopic adhesiolysis. Common to all pathologies is the involvement of 3rd site in the AP regioumbilicalis, because it is projection of the small intestine loops, which are most vulnerable to the AP.
The most interesting group consisted of 11 children who underwent surgery for recurrent AIO. Before surgery, 2 children underwent 4 relaparotomy, 4 children: 3 relaparotomy, 3 children: 2 relaparotomy and 2 children: 1 relaparotomy. In previous surgeries, all children underwent total adhesiolysis without the use of barrier solutions. 5 patients underwent small bowel resection (1 stoma removal due to severe condition of the child, 4 small bowel resection with anastomosis), in 1 case small bowel intubation with Abbott-Miller probe.
During the operation, in this category of patients, it was impossible to establish the primary location of the AP, because there were all types of adhesions with spread to the entire abdominal cavity and projection on all parts of the abdominal wall. Thus, relaparotomies contribute to the further development of the AP.
When observing children for 15 years, the recurrence of AIO was observed according to (Table 6).
| Surgical interventions | Main group | Comparison group | ||
|---|---|---|---|---|
| Adhesiolysis | 12 | 2 | 13 | 4 |
| Adhesiolysis and resection of the small intestine | 6 | 1 | 4 | 1 |
| Adhesiolysis with ileostomy | 1 | - | 1 | - |
| Elimination of the cause without total adhesiolysis | 12 | - | 13 | 1 |
| Elimination of the cause without total adhesiolysis and resection of the small intestine | 6 | - | 3 | 1 |
| Elimination of the cause without total adhesiolysis and ileostomy | 1 | - | 1 | - |
| Total | 38 | 3 (7.89%) | 35 | 7 (20%) |
Table 6: Distribution of children with LAIO, according to the performed surgical interventions and recurrence of the disease (n=73). In the main group of patients recurrent AIO was resolved conservatively, in the comparison group 4 of 7 children required relaparotomy. The operated children used the method of eliminating the cause of AIO without total adhesiolysis using sodium hyaluronate. When children were observed for 1 to 7 years, recurrence of AIO was in 1 patient who resolved conservatively.
Thus, the development of adhesions of the abdominal cavity trigger is damage to the mesothelium, which occurs: mechanically (during surgery), due to irritating action, which triggers the mechanisms of the immune response (peritoneal dialysis, installation of drainage) and inflammation. AP occurs primarily at the site of mesothelial damage and is able to spread to surrounding areas and structures of the abdominal cavity, while projecting to different parts of the abdominal wall.
Total adhesiolysis leads to recurrence of AIO to a greater extent than surgery to eliminate the cause without adhesiolysis. The usage of sodium hyaluronate in combination with decamethoxine acts on the pathogenetic links of the formation of adhesions, reducing the number of relapses. Sodium hyaluronate is an active substance that is present in the extracellular matrix, and decamethoxime is an effective antimicrobial agent. Thus, sodium hyaluronate has a barrier function up to 3 days while mesothelial wounds heal and decamethoxine inhibits microbial activity, helps to reduce the density and number of adhesions.
Conclusion
Damage to the mesothelium leads to the primary AP of the abdominal cavity with the spreading to the surrounding structures and projection on the areas of the anterior abdominal wall. The use of abdominal cavity drainages in children provokes the development of AP, so it should be limited and performed only under strict indications.
Adhesion conglomerates (32.88%) and moorings (23.28%) are the most common causes of relaparotomies in LAIO in children. In operations on LAIO in children, it is advisable to use the operation of eliminating of the cause (separation or resection of the conglomerate, cutting of the «mooring») without providing of total adhesiolysis in combination with intraoperative use of sodium hyaluronate solution with decamethoxine.
The projection of the AP on the anterior abdominal wall, depending on the previous operation in children can be used at laparoscopic surgeries performing.
References
- Catena F, DiSaverio S, Coccolini F, et al. Adhesive small bowel adhesions obstruction: Evolutions in diagnosis, management and prevention. World J Gastrointest Surg 2016; 8(3):222–231.
- Aref- Adib M, Phan TS, Ades A. Preventing adhesions in laparoscopic surgery: the role of anti- adhesion agents. Obstet Gynecol 2019; 21:185 - 192.
- Tabibian N, Swehli E, Boyd A, et al. Abdominal adhesions: A practical review of an often overlooked entity. Ann Med Surg 2017; 15:9–13.
- Correa-Rovelo JM, Villanueva-López GC, Medina- Santillan R, et al. Obstrucción intestinal secundaria a formación de adherenciaspostoperatorias en cirugía abdominal. Revisión de la literatura Intestinal obstruction secondary to postoperative adhesion formation in abdominal surgery. Review. Cir Cir 2015; 83(4):345–351.
- Vogels RR, Bosmans JW, van Barneveld KW, et al. A new poly(1,3-trimethylene carbonate) film provides effective adhesion reduction after major abdominal surgery in a rat model. Surgery 157(6):1113–1120.
- Macarak EJ, Lotto CE, Koganti D, et al. Trametinib prevents mesothelial-mesenchymal transition and ameliorates abdominal adhesion formation. J Surg Res 2018; 227:198–210.
- Krielen P, Grutters J, Strik C, et al. Cost-effectiveness of the prevention of adhesions and adhesive small bowel obstruction after colorectal surgery with adhesion barriers: a modelling study. World J Emerg Surg: WJES 2019; 14:41.