Current Pediatric Research
International Journal of Pediatrics
Restoring esthetics and function with multidisciplinary dental management in a girl child with special needs.
Pedodontics and Preventive Dentistry, Bharati Vidyapeeth Deemed University Dental College, India.
- *Corresponding Author:
- Anil Patil
Associate Professor, Pedodontics and Preventive Dentistry
Bharati Vidyapeeth Deemed University Dental College
Sangli, Maharashtra, 416414, India.
Tel: +91 9850983500
E-mail: dranilp0888@gmail.com
Accepted date: April 05, 2017
This case report describes the multidisciplinary treatment of a 14 year old girl whose Class I malocclusion treatment was complicated by her deaf and dumbness. The need to provide aesthetic as well a functional dental occlusion for special child continues to be a challenge for the Orthodontist despite proper preoperative evaluation and good rapport building with the patient. We would like to emphasize on preoperative Rapport building and use of simple sign language for conduct of dental treatment safely and effectively. On intra-oral examination it showed bi-maxillary protrusion on account of Angle’s Class I malocclusion with maxillary and mandibular anterior spacing and proclination. There was Elli’s Class I fracture with 11 and 21, short clinical crowns with increased incisal and gingival display during smile was seen. Complete oral rehabilitation was done on the dental chair, keeping appointments short by using four-handed dentistry. The patient is currently on a semi-annual periodic recall since one and a half years and continues to show satisfactory oral health.
Keywords
Deaf, Dumb, Four handed dentistry, Orthodontic treatment, Special child, Sign language.
Introduction
The special children and adolescents appear to have poorer oral health than their normal counterparts. When oral health has lots of importance in general health of children, in special children pressing medical issues often take focus and dental care takes back seat. Oral hygiene has strong biological, physiological and psychological basis that’s why it affects esthetics and communication [1].
As Individuals with Special Health Care Needs encompasses a wide variety of physical, developmental, mental, sensory, behavioral, cognitive, and emotional impairments they require medical management, health care interventions, and/or use of specialized services or programs. These children present a special challenge to the dental health care team. It is generally acknowledged that majority of disabled children have been dentally neglected [2]. Children with special needs exhibit a higher percentage of malocclusions and craniofacial deformity. This is related to more frequent abnormal growth and development, higher incidence of abnormal tongue posture and orofacial muscular disturbances [3]. Despite the recognition that dental professionals can play an important role in the rehabilitation of these children, many dentists are reluctant to treat these children. The dentists they may refuse to treat these children because of lack of knowledge, fear and anxiety regarding the disability and unfamiliarity with the techniques required for their dental care. Deaf mutism is a major health problem and limits appropriate communication and learning that is necessary for the normal development and maturation. We are presenting a multidisciplinary dental treatment of a deaf and dumb girl.
Case Report
A 14 year old deaf and dumb female patient reported to the private orthodontic clinic complaining of spacing and forwardly placed upper front teeth, her parents expressed difficulty in chewing and increased tooth and gum display during smile. The parents and the patient both were very concerned and eager to get the Orthodontic and other dental treatment done for improving esthetics as she was about to participate in the Special Olympics World Summer Games, held in Los Angeles, California in July 2015. The family history revealed that the parents had consanguineous marriage and her younger brother was also deaf and mute congenitally.
A) Medical history and records revealed that the patient is deaf and dumb since birth. All the development milestones were delayed in the child. The patient was of average built, height 145 cm, weighed 36 kg and walked with a normal gait. Might be because the patient was swimmer in spite of diagnosed as handicapped child by specialist health professionals she was very enthusiastic and very well oriented. The healthy workout of swimming could provide endurance, muscle strength, and cardiovascular fitness for her. Other routine investigations were normal. B) Intraoral examination showed high arched palate, macroglossia and malocclusion was Class I. Preoperative visit focused on educating and interacting with patient and parents. Girl was taught to express pain by showing the Visual Analog Pain Scale (VAS) during treatment. The girl was reassured and a mock trial of the sign language was done to assess the understanding of the girl.
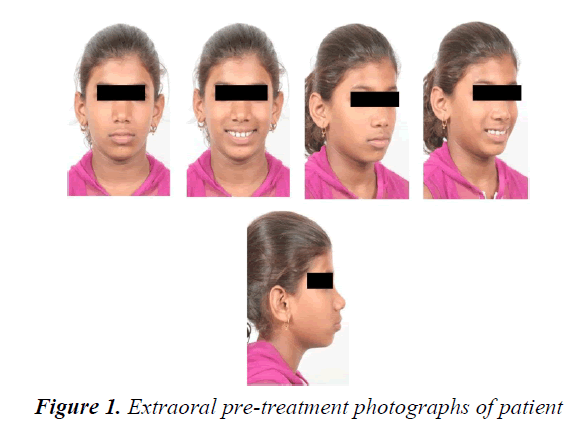
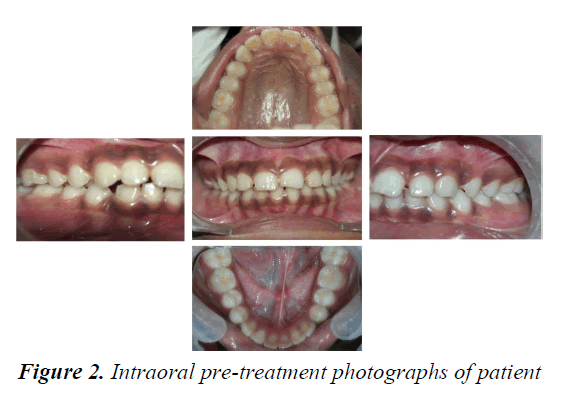
Extra-oral examination revealed convex profile with protrusive upper and lower lips, acute nasolabial angle and deep mento-labial sulcus (Figure 1). Intra-oral examination showed bi-maxillary protrusion on account of Angle’s Class I malocclusion with maxillary and mandibular anterior spacing and proclination. The Elli’s Class I fracture with 11and 21, short clinical crowns with increased incisal and gingival display during smile was seen. The hyper pigmented gingiva is seen during smile (Figure 2). On radiographic examination there was presence of all 32 permanent teeth with the 3rd molars unerupted and mild spacing .The cephalometric analysis confirmed the Class I bi-maxillary protrusion as SNA of 87 0 and SNB of 850, proclination of the upper incisors (U1 to Mx Plane 130°) and lower incisors (L1 to Md Plane 105°). The soft tissue examination confirmed protrusive upper and lower lips and impaired facial esthetics.
Treatment Objectives for Four-Handed Dentistry
Integrated Conservative, Oral Surgery, Orthodontic, Periodontal treatment objectives were established as shown in following Table 1. The ultimate objective was to achieve an esthetic and functional occlusion.
Treatment Progress
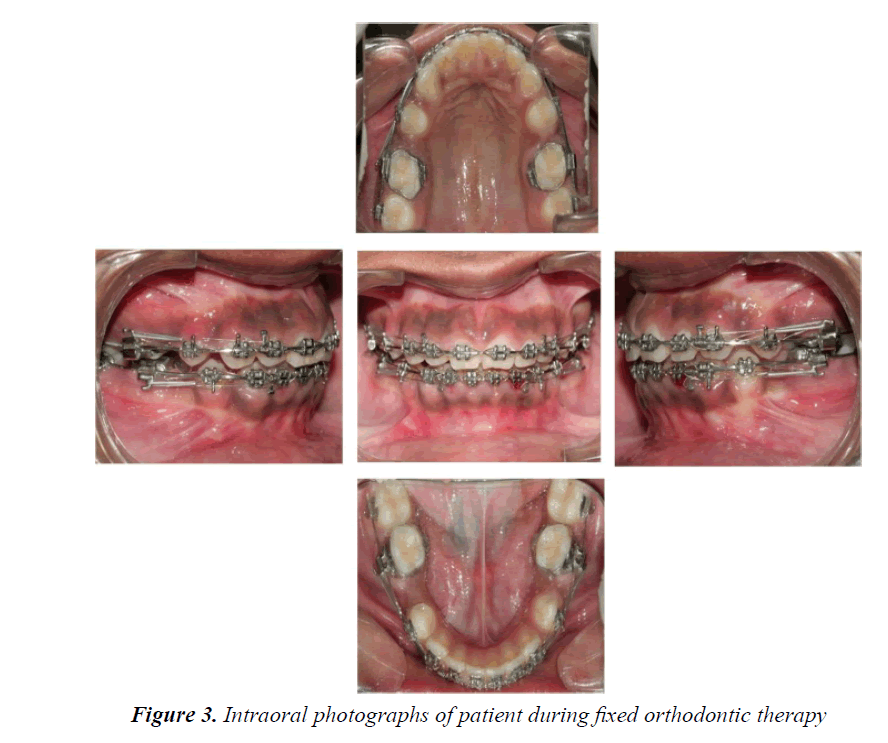
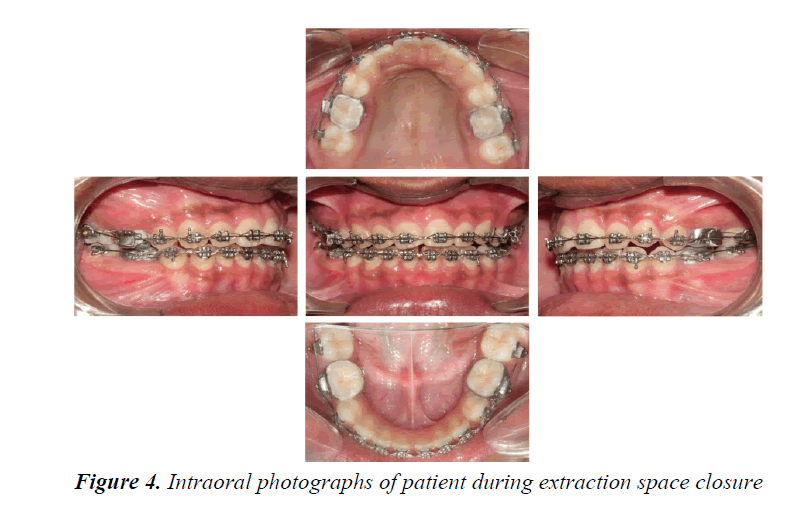
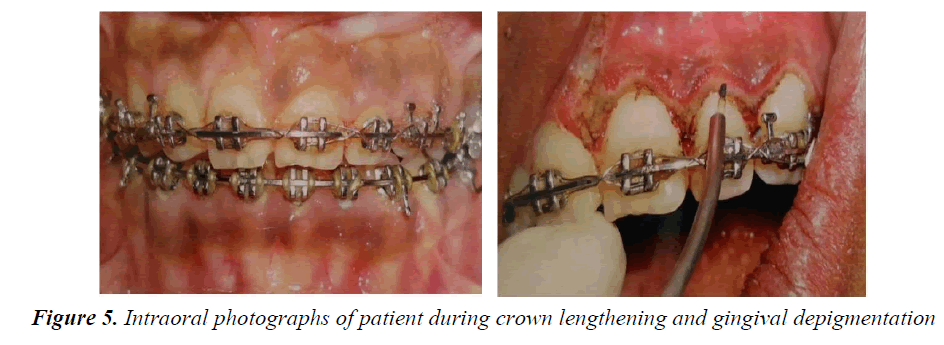
The strap up was done using 0.022 MBT prescriptions. All the teeth were bonded in the upper and lower dental arches except the second molars. The bonding was done according to MBT recommendations. The fractured incisal edges were restored with composite esthetic build ups before bonding which are used as reference for anterior teeth and the inter-marginal ridge lines of premolars and molars for the posterior teeth (Figure 3). As there was no upper or lower crowding, the initial alignment was performed with 0.014”NiTi arch wires and subsequently 0.016”NiTi. This is useful for the correction of any remaining rotations after the initial alignment. Leveling was achieved with 0.019”/0.025”NiTi wires. The therapeutic extractions of all second premolars were performed at the end of the leveling and alignment stage under conscious sedation and local anesthesia. The second molars were bonded before space closure to reinforce the anchorage; no other anchorage control measure was used. Spaces were closed using active tie backs on rectangular 0.019”/0.025” steel wires with hooks welded to the mesial of canines (Figure 4). Following space closure generalized gingivectomy under conscious sedation targeted to crown lengthening was carried out (Figure 5). Periodontal dressing was given to cover the surgical site. Routine postoperative instructions were given. The medications prescribed were, tablet Amoxicillin 250 mg and tablet Paracetamol 500 mg three times a day for 5days.
| Treatment Objectives | Treatment Plan |
|---|---|
| Conservative Objectives |
•Restore fractured teeth •Restore carious teeth |
| Â Oral Surgery Objectives | •Therapeutic extractions of all four second premolars |
| Orthodontic Objectives |
•Reduce the bi-maxillary proclination •Obtain class I canines with good anterior guidance •Improve the overbite •Maintain class I molars •Improve the facial esthetics with a more balanced Upper and lower lips. |
| Periodontal Objectives |
•Oral Prophylaxis •Generalized crown lengthening •De-pigmentation of gingiva |
Table 1. Integrated treatment objectives and treatment plan
As Conscious sedation is a Pharmacologically-induced state of relaxation in which the patient remains conscious, it was induced while treating the patient. It was helped in changing patient’s mood and degree of compliance throughout the dental treatment, facilitating acceptance of the procedure as she was frightened patient. Conscious sedation has opened the way for the dentist to provide treatment for special child in some of the most resistant aspects like surgery and extractions - previously considered untreatable.
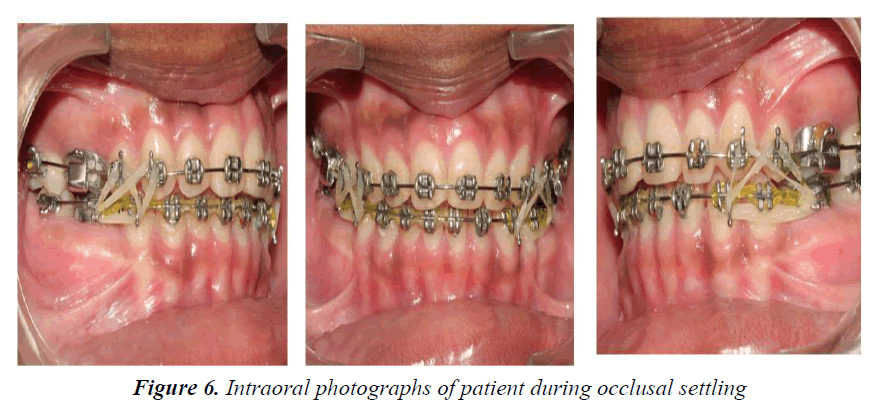
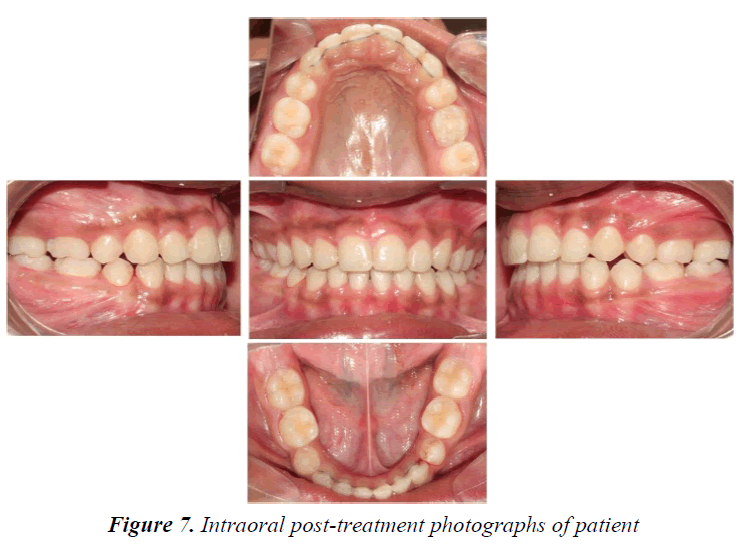
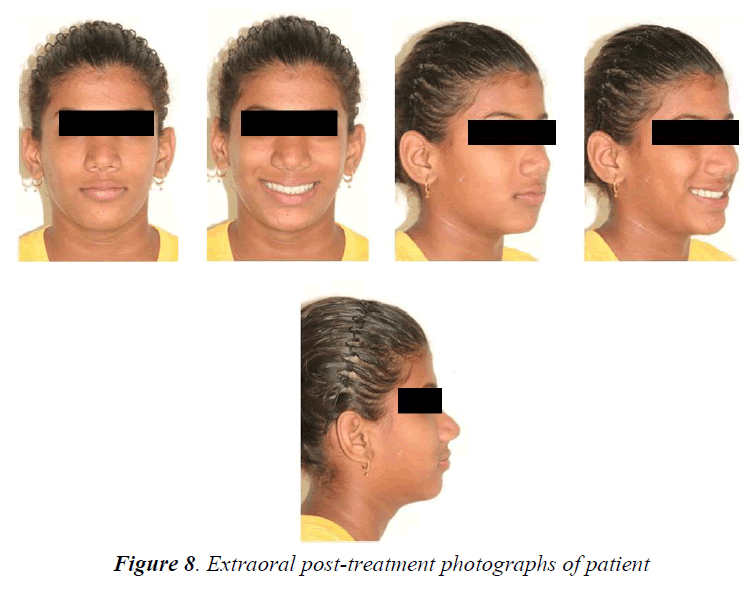
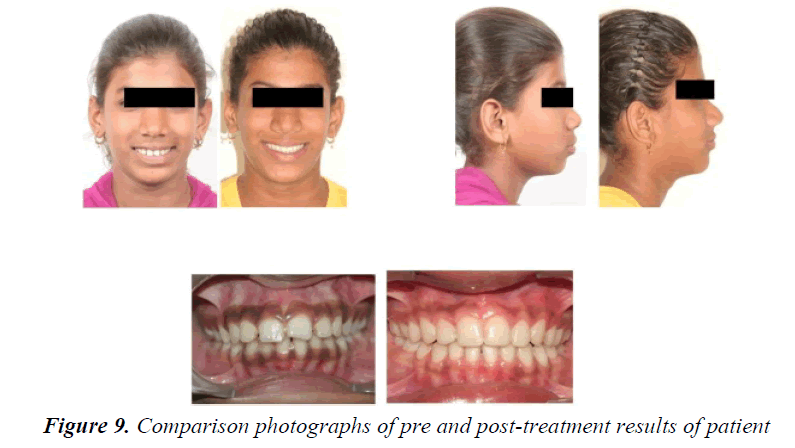
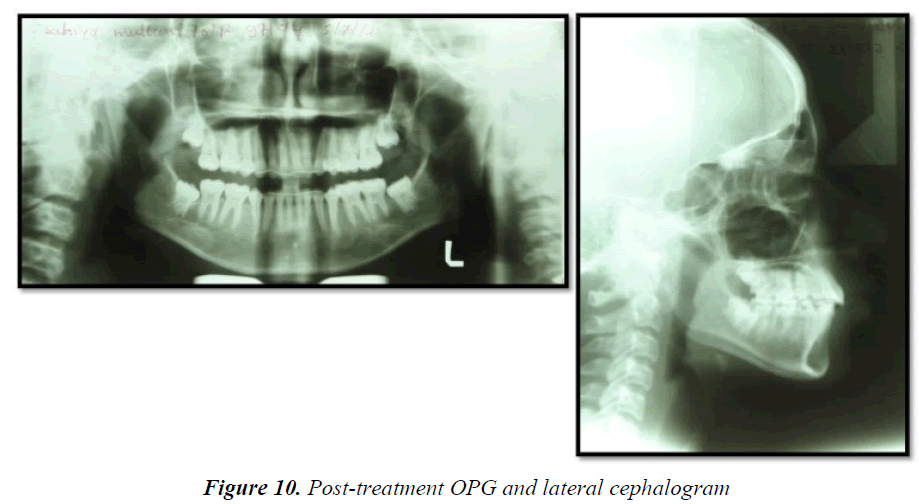
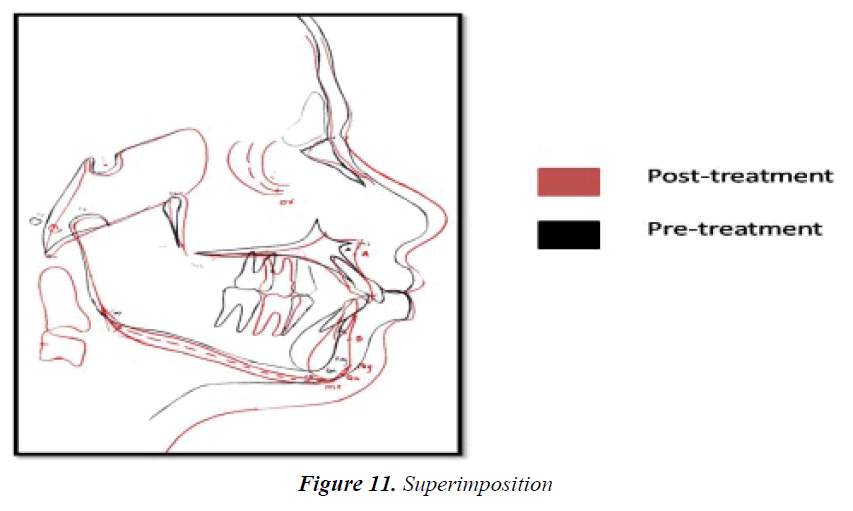
Crown-lengthening procedure helped to improve the results of orthodontic treatment. Clinical crown lengthening was based on the adequacy of a biological width of 2.04 mm in order to obtain healthy periodontal tissue. Patient has taught to place settling elastics for a period of 2 months for finishing and detailing (Figure 6). During the finishing and detailing the closed spaces were maintained with passive lace backs under the arch wire from second molar to second molar. The fixed appliance was removed after ensuring a perfect intercuspation of the teeth and good functional movements after 14 months of commencement of treatment (Figures 7-9). At this stage, a fixed 3/3 lingual retainer was bonded to the upper and lower arch. The Hawley retainer was prescribed for a period of 6 months full time and after 6 months night time wear. The upper and lower 3/3 lingual retainer will be kept in place for a period of 2 years. The satisfactory treatment results were achieved. There was controlled mesial movement of molars. Spacing in the anterior was corrected. There was retraction and up righting of incisors to a more favorable position and also there was improvement of facial profile. Protrusion of the upper and lower lips was reduced (Figures 10 and 11).
Discussion
This case highlights some important issues related to deaf and dumb child that are relevant for all orthodontists as well as general dentists. First, the clinician must be able to identify special children and their needs. The ability to identify and quantify malocclusion in special children poses a challenge to the clinician. Special children definitely have special orthodontic need in comparison to their normal counterparts and require similar attention and treatment without prejudice and discrimination [3]. Strict standard norms should not be adhered to while assessing treatment needs and rendering treatment to patients with special needs. Patient’s appropriate concerns and expectations must be taken into consideration during assessment of severity of malocclusion and determining treatment needs for a particular patient [4]. The prevalence and severity of malocclusion is especially high in special needs individuals. They often present with the medical limitations to the various procedures which are required to achieve desirable orthodontic treatment outcome. This is further complicated by presence of moderate to severe behavioral problems that make treatment delivery even more challenging [5]. Treating these patients are extremely demanding and are not for everyone! The deaf are those in whom the sense of hearing is nonfunctional for the ordinary purposes of life. This general group is made up of two distinct classes based entirely on the time of loss of hearing. The congenitally deaf are those who are born deaf and the acquired ones are those who are born with normal hearing but the sense of hearing became nonfunctional later through illness or accident [6].
According to equilibrium theory the teeth are positioned in the dental arch between the opposing forces of the lips and tongue. However, additional forces or tonus changes either from tongue or lips to the teeth over extended periods of time will upset the equilibrium of the dental arch, creating a malocclusion [6]. The research proposed that deaf-mute individuals do not displace their tongue as it is less flexible than that of normal hearing individuals in order to establish vowel steady-state postures to establish the equilibrium [7]. Considering this difference, the present case report addresses the management of occlusal discrepancies of deaf-mute child by multidisciplinary approach. Since its difficult to predict the time required for their scheduled work they may disturb the regular clinic schedule times thus may require additional number of appointments [8]. Since the availability of several professionals like Pedodontist, Endodontist, Oral surgeon, and Anesthetist is rarely found in a private clinic, being usually achievable only in a hospital-type of setting Majority of dental procedures could be performed under conscious sedation in a single sedation session [9]. Dental surgeons and paramedical staff they had little training or experience in handling such special situations which include preoperative familiarization with the patient and her family. Parental presence is highly desirable during induction of sedation [10]. In the present case report the multidisciplinary dental management was carried out in the dental clinic itself once the good rapport and cooperation of a patient was gained.
Development of deaf child varies significantly from normal child. Therefore, the child should not be treated as being like routine patient, because deafness has definite and unique consequences on the personality of a developing child, resulting from difficulty in communicating with others [11]. If possible, the dental appointment should be scheduled so that the patient spends little time in the waiting room. When the child is seated in the dental chair the dentist, assistant, and parent are all should be positioned such that the patient can easily view them. The parents were visible for interpretation and reassurance. However, the dentist and assistant could easily convey ideas to the deaf child through gestures, facial expressions and slow pronunciation of words [12]. Generally children like body contacts like patting on the shoulder or handshaking, as positive reinforcement for good performance, and the deaf child is no exception to it. Once a good rapport is gained between patient and dentist, the child gains a sense of security and confidence decreasing the importance of the parent’s presence. Eventually, as successive appointments continued, the child gained a sense of independence and often willfully desired to get treated. Fortunately the parents of the deaf patient were not overprotective thus the Temper tantrums, lack of cooperation did not evoke sympathy from the parent disturbing the treatment [13]. All the instruments and equipment, that is, the air, water spray, the air rotor and others were demonstrated for the deaf child. The vibrations of the equipment which the child felt were been previously explained as normal and to be expected in the dental office. The deaf child is especially fearful of the unknown; therefore, maximum number of demonstrations and explanations would be most beneficial. Actual dental treatment for deaf child was closely paralleled with treatment of hearing child only the extensive preventive program should be initiated, as deaf children often exhibit poor oral hygiene. Parents often appease their children by rewarding them with excessive candy and sweets which should be discouraged. Need for corrective home care measures and nutritional guidance should be emphasized to the parents [14].
The therapeutic extractions and the crown lengthening were performed under conscious sedation and local anesthesia. In order to gain patient co-operation, it was essential to explain the concept of local anesthesia in a way that the child could understand it before beginning of procedure. Parents would be helpful in interpreting this procedure to their child by describing the fact that the teeth will be asleep. Substitute for the word “hurt” had often proved ineffective, once the local anesthetic had been administered, it was imperative that the oral surgeon and periodontist be absolutely positive that it had taken effect. Crown lengthening was performed as of Cohen’s concept which is presently a procedure that often involved a combination of soft tissue removal and osseous surgery during orthodontic treatment for tooth exposure. One important factor should be considered during crown lengthening is amount of attached gingiva. It has been shown that to maintain periodontal health there should be 2-3 mm of attached gingiva [15]. Restorative treatment procedures were performed without complete anesthesia; however, during treatment patient had often regressed in behavior and had become a management problem. The most important treatment objective was to improve the alignment and occlusion of the teeth and thus, indirectly, this resulted in improvement of facial appearance. However, its reliability is questionable and it cannot provide a satisfactory answer for every situation.
Emphasis should be placed on the use of sign language in handling such cases; this can reduce fundamental misunderstandings while interacting with the patients. In the Indian deaf population of 3.1 million, 98% are illiterate thus sign language can be used effectively in deaf and dumb for any complex procedure which needs full patient co-operation and support thus felicitating successful outcome [16].
According to a study conducted on handicapped children of Calcutta, India it was reported that dental caries incidence was highest in mentally retarded children followed by cerebral palsied, blind, epileptic, physically handicapped, children with Down's syndrome and deaf and dumb. The caries prevalence of handicapped children was higher than the normal children [17]. Intravenous Sedation (IVS) is useful for the dental treatment of patients with intellectual disability. However, in obese patients, special care should be taken during intravenous sedation as difficulties in airway management can easily lead to oxygen desaturation leading to complications [18]. Various researches have assessed the orthodontic treatment needs of the handicapped population and the response of different orthodontic treatment centers to this need using Treatment Priority Index (TPI). It was found that 40.3% had normal occlusions, 21.5% had slight malocclusions, 25.2% had malocclusions that required treatment, and 5.0% had severe malocclusions. The aim of orthodontic treatment for patients with disability must be modified from the conventional goals. While treating such patients the Orthodontist should focus on esthetically acceptable and functional treatment results rather than striving for orthodontic perfection. Sometimes this requires an ability to select less conventional treatment plans. The ability to identify and quantify malocclusion in special children poses a challenge to the clinician. Special children definitely have special orthodontic needs in comparison to their normal counterparts and require similar attention and treatment without prejudice and discrimination.
Conclusion
An orthodontist must be able to identify various special health conditions and their possible impact on treatment procedures. The primary treatment goal should be preparing good rapport with the patient before starting with the treatment. Treatment should be appropriately postponed until the underlying medical problem is addressed or the side effects of the drug therapy are minimized. Comprehensive treatment may not always benefit the patient. Treatment procedure should be modified according to patient need. Consent before treatment, good patient cooperation and constant monitoring of the progress of the treatment are necessary to minimize physical damage and to maximize treatment outcome. The practitioner must be aware of the psychological aspects of the child’s handicap and the strong dependence that the child has on the parent. When the dentist understands these aspects, he will be attuned to the situation he is facing and will be able to effectively overcome the communication gap between the patient and him. Once this occurs and the clinician gains complete confidence of his patient, he will discover that performing dental care for the deaf child is the most rewarding and satisfying experience.
References
- Mistsea AG, Karidis AG, Bakoyianni D, et al. Oral health status in Greek children and teenagers with disabilities. J Clin Pediatr Dent 2001; 26: 111-118.
- Crall JJ. Improving oral health for individuals with special health care needs. Pediatr Dent 2007; 29: 98-104.
- Maurya R, Naik H, Kalra A, et al. Determination of dentofacial deformities and orthodontic treatment requirement in differentially abled children using IOTN. Int J Oral Health Dent 2015; 1: 120-124.
- Suma G, Das UM, Akshatha BS. Dentition status and oral health practice among hearing and speech-impaired children: A cross-sectional study. Int J Clin Pediatr Dent 2011; 4: 105-108.
- Singh RK, Murawat K, Agrawal R. Dental care for the deaf pediatric patient dental care for the deaf pediatric patient. Indian J Otol 2012; 18: 171-173.
- Graber TM. The three M: Muscles, malformation and malocclusion. Am J Orthod 1963; 49: 418-450.
- Murray NT. The establishment of open articulatory postures by deaf-mute and hearing talkers. J Speech Hear Res 1991; 34: 453-459.
- Arora1 A, Prakash A. Orthodontic management in children with special needs. Int J Med Dent 2013; 3: 207-211.
- Becker A. Orthodontic treatment of disabled children. J Orthod 2001; 28: 39-44.
- Becker A. Behavior management needs for orthodontic treatment of children with disabilities. Eur J Orthod 2000; 22: 143-149.
- Bowen DI. Collum LMT, Rees DO. Clinical aspects of oculo-auriculo-vertebral dysplasia. Br J Ophthalmol 1971; 55: 145-154.
- Myklebust HR. Auditory disorders in children. New York: Grune and Stratton. 1954.
- Miller JB. Dental care for the deaf child. J Okla State Dent Assoc 1970; 60: 38-42.
- Cigera S, Akanb S. Occlusal characteristics of deaf-mute individuals in the Turkish population. Eur J Dent 2010; 4: 128-136.
- Maynard JG, Wilson RDK. Physiological dimensions of the periodontium significant to the restorative dentist. J Periodontol 1979; 50: 170-177.
- Goyal S, Sharma I, Sharma S. Sign language recognition system for deaf and dumb people. Int J Eng Res Technol 2013; 2: 382-387.
- Gupta DP, Chowdhury R, Sarkar S. Prevalence of dental caries in the handicapped children of Calcutta. J Indian Soc Pedod Prev Dent 1993; 11: 23-27.
- Onishi R, Higuchi H, Kawase A. Airway management using a nasal high flow system (Optiflow?) during intravenous sedation for dental treatment in an obese patient with intellectual disability. Journal of Japanese Dental Society of Anesthesiology 2016; 44; 207-209.