Current Pediatric Research
International Journal of Pediatrics
Misdiagnosis of pneumonia, bronchiolitis and reactive airway disease in children: A retrospective case review series in South East, Nigeria.
1Faculty of Medical Sciences, University of Nigeria, Ituku-Ozalla, Enugu State Nigeria.
2College of Medicine, Enugu State University of Science and Technology, Nigeria.
3Federal Medical Center, Umuahia, Nigeria.
- Corresponding Author:
- Egbuna Obidike
Professor of Pediatrics, University of Nigeria, Faculty of Medical Sciences
Ituku-Ozalla, Enugu State, Nigeria
Tel: 234-803-321-9404
Email: egbunaobidike@yahoo.com
Accepted date: June 20th, 2018
Background: Pneumonia is a major cause of morbidity and mortality in children especially in sub Saharan Africa and Asia. Recent studies suggest that pneumonia may be overdiagnosed at the expense of other acute respiratory conditions with similar features such as asthma and other wheezy conditions, and bronchiolitis. This study examined the prevalence and diagnostic concordance of hospital diagnoses made with an established Case Definition Criteria (CDC) for these three common respiratory disorders in the south east region of Nigeria Materials and Methods: Hospital admission records of all children aged between 2 and 59 months who presented with, catarrh, respiratory distress, cough and fever between January and December 2015 in the children emergency room of three hospitals in South East Nigeria were reviewed. Results: A total of 186 case records met the inclusion criteria and were analyzed. Bronchopneumonia accounted for 41.9%, of the cases admitted; while reactive airway disease and bronchiolitis accounted for 16.1% and 9.1% respectively based on the hospital diagnoses, and 33.3%, 23.1% and 5.9% respectively using the case definition criteria. The positive and negative predictive values for diagnosing bronchopneumonia (BP) were 72% and of 94% respectively. For reactive airway disease (RAD), the values were 57% and 83% respectively while that for bronchiolitis (BL) were 53% and 99% respectively. Conclusion: There is need for a review of the criteria for diagnosis of these respiratory conditions in children that are similar to forestall the danger of misdiagnosis and inappropriate treatment of children with these conditions.
Keywords
Respiratory diseases, Under fives, Southeast Nigeria.
Introduction
Respiratory diseases are common feature in paediatric practice [1,2]. They are often infective or reactive but the infective causes are said to be more common [1,3]. Of these infective causes, morbidities and mortalities have been most associated with pneumonia especially in low-income countries [3,4]. These morbidities and mortalities have also been noted to be adversely affected by some factors such as age, state of nutrition, presence of co-morbid conditions in the affected children etc [1-3,5]. Some efforts at finding ways of identifying the child with pneumonia have led to a number of ways of classifying the child with respiratory diseases and case definitions [6-9]. The recently revised clinical guideline for childhood pneumonia diagnosis by the World Health Organization considers pneumonia in a child with or without fever presenting with cough and difficulty in breathing/lower chest in-drawing at the firstlevel health facility and outpatient department [6]. There are however other conditions with similar clinical features that may not have been excluded in the definition used for pneumonia. It becomes worrisome the implication of diagnosing every child with cough and fast/difficult breathing with or without fever as pneumonia. This is more so when it is realized that achild with RAD and with any cause of fever, especially malaria, the common cause of fever in our environment, will present with similar symptoms in a co-morbid state. This diagnostic dilemma has also been noted in publications [10-12].
These studies have suggested that lack of clearly defined case definition and poor recognition of these conditions which mimic pneumonia in children may have unduly increased the figures ascribed to pneumonia [11,12]. This research set out to verify the dominant school of thought that pneumonia is responsible for most of the morbidities attributable to respiratory disease in under five children in our area. The study reviewed the prevalence, pattern, demography and diagnostic concordance of hospital diagnoses made with an established Case Definition Criteria (CDC) for the three common respiratory diseases with potentially similar clinical signs in 2-59 months old children from three hospitals in the south east region of Nigeria and has been designed in such a way as to throw up facts that will add to knowledge about these conditions in the area.
Materials and Methods
A case series analysis of all respiratory cases that presented in the children emergency units of the University of Nigeria Teaching Hospital (UNTH), Ituku/Ozalla, Enugu, ESUT/ Park Lane Teaching Hospital Enugu and Federal Medical Center Umuahia over a one year period (January 2015 to December 2015) was done. The University of Nigeria Teaching Hospital (UNTH) Ituku-Ozalla and Enugu State University Teaching Hospital (ESUT) Park Lane Enugu are teaching hospitals in Enugu State serving inhabitants of Enugu metropolis, its environs and sometimes surrounding states. On the other hand, Federal Medical Center Umuahia serves the inhabitants of Umuahia and its environs in Abia State. All the centers are in Southeast Nigeria.
The hospital admission records of all children aged between2 and 59 months who presented with, catarrh, respiratory distress and or cough and or fever between January and December 2015 in the children emergency room of the three hospitals were reviewed. Those of them who had bronchopneumonia (BP), reactive airway disease (RAD), and bronchiolitis (BL) as the final diagnosis or as a co-morbid state were selected.
Data from all admission records of cases selected for the study were retrieved and the information on admission in the records of those cases with final diagnoses of BP, RAD and BL were extracted. These included patient demography and clinical features.
Furthermore, data from the case records were reviewed using the CDC that were developed from standard clinical approach to diagnosis and WHO guidelines designed for this research (see Definitions) [7].
Ethical approval for the study was obtained from the Health Research and Ethics Committees of the three hospitals Information obtained from the case notes were treated as confidential.
Data Management
Data obtained was entered into Microsoft Excel® (2010, Microsoft Corporation, Redmond Washington USA) and analyses subsequently done with Statistical Package for Social Sciences (SPSS) version 20 (2011, IBM Inc. Chicago Illinois, USA). Shapiro Wilk's W test was used to check normality of various variables. Test of association between variables were done using the chi-square test for nominal variables. Sensitivity and specificity and predictive values of the final hospital diagnosis and the CDC based diagnosis were determined. Statistical significant value was set at a p value of ≤0.05 with confidence interval of 95%.
Definitions
The case definitions were developed from standard clinical approach to diagnosis and WHO guidelines [7]. designed for this research.
Reactive Airway Disease
Children whose clinical presentations were that of cough, tachypnoea, dyspnoea, wheeze, with or without hyperresonance were classified as having ‘reactive airway disease’. This is an umbrella term used in this study to categorize all wheezy children inclusive of those diagnosed to have asthma following the Global Initiative for Asthma (GINA) guideline but exclusive of bronchiolitis. The presence of any four of above features were considered diagnostic. Terminologies such as bronchitis, bronchitisasthma, wheezing disorder and hyper-reactive airways disease, have been used to describe children with cough and wheezing [13].
Bronchiolitis
A child with any five of coryza, tachypnoea, dyspnoea, wheeze, hyper-resonance, crepitations, with or without fever was classified as a case of bronchiolitis.
Pneumonia
A child was said to have pneumonia if he had the following symptoms/signs/laboratory features: fever, new onset of worsening cough, dyspnoea, tachypnoea, crepitations or bronchial breath sounds, Leucopenia (<4000 wbc/mm3) or leucocytosis (≥ 12000 wbc/mm3) with or without chest X-ray showing features in keeping with pneumonia. Any three of the clinical features inclusive of crepitations was considered as diagnostic.
Rapid Diagnostic Test (RDT) positivity was also sought for in all these when there is a fever.
Results
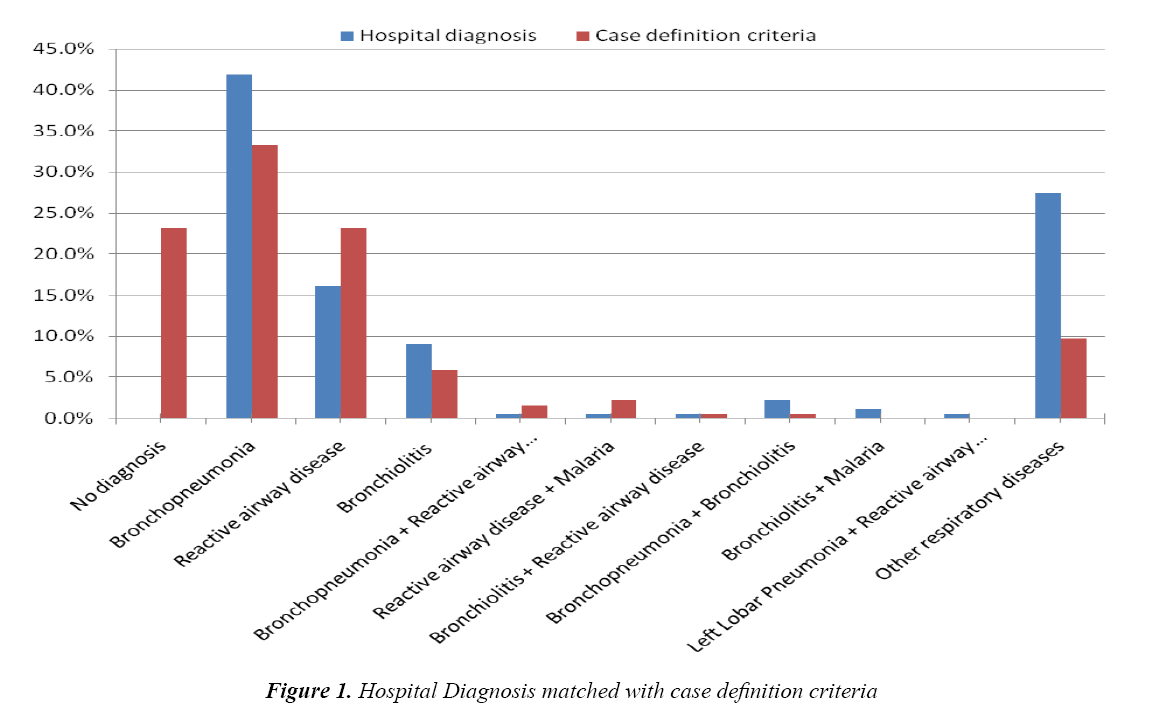
Due to paucity of laboratory results, this study relied mostly on the clinical bases for diagnoses made and used such when matching findings with expectations. A total of 196 case records were reviewed. Of these 10 cases did not meet the criteria and were excluded: five had incomplete data entries, three were cases of HIV/AIDS, one had multiple diagnoses and one did not have a definite diagnosis (Figure 1).
Table 1 shows that age of presentation showed a significant difference between the three diseases in both groups while in Table 2, there is no significant difference in sex presentation in the three diseases, whether as hospital diagnosis based or case definition criteria based.
| BP | RAD | BL | P Value (Kruskalwallis) | |
|---|---|---|---|---|
| Median | Median | Median | ||
| Hospital Diagnosis (Age (months)) |
9 | 25 | 4 | < 0.001 |
| Case Definition Criteria (Age (months)) |
9 | 13 | 4 | 0.011 |
Table 1: Median age distribution of cases
| BP | RAD | BL | P value | ||
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | |||
| a. Hospital Diagnosis | |||||
| Sex | |||||
| Male | 45 (61.6) | 20 (27.4) | 8 (11.0) | 1.76 | 0.415 |
| Female | 33 (63.5) | 10 (19.2) | 9 (17.3) | - | - |
| a. Case Definition Criteria | |||||
| Sex | |||||
| Male | 35 (55.6) | 23 (36.5) | 5 (7.9) | 0.525 | 0.769 |
| Female | 27 (50.0) | 21 (38.9) | 6 (11.1) | - | - |
Table 2: Sex prevalence of bronchopneumonia, reactive airway disease and bronchiolitis
From Table 3, the predominant respiratory diagnoses were bronchopneumonia-41.9%, reactive airway disease-16.1% and bronchiolitis-9.1%. Using the case definition criteria, the prevalence of bronchopneumonia was 33.3%, reactive airway disease and bronchiolitis 23.1% and 5.9% respectively. Other respiratory disease cases were aspiration pneumonitis, foreign body aspiration, upper respiratory tract infection, severe malaria anemia and sepsis presenting with respiratory distress.
| Hospital Diagnosis | Case Definition Criteria | |
|---|---|---|
| n (%) | n (%) | |
| No diagnosis | - | 43 (23.1) |
| Bronchopneumonia | 78 (41.9) | 62 (33.3) |
| Reactive airway disease | 30 (16.1) | 43 (23.1) |
| Bronchiolitis | 17 (9.1) | 11 (5.9) |
| Bronchopneumonia + Reactive airway disease | 1 (0.5) | 3 (1.6) |
| Reactive airway disease + Malaria | 1 (0.5) | 4 (2.2) |
| Bronchiolitis + Reactive airway disease | 1 (0.5) | 1 (0.5) |
| Bronchopneumonia + Bronchiolitis | 4 (2.2) | 1 (0.5) |
| Bronchiolitis + Malaria | 2 (1.1) | 0 (0.0) |
| Left Lobar Pneumonia + Reactive airway disease | 1 (0.5) | 0 (0.0) |
| Other respiratory diseases | 51 (27.4) | 18 (9.7) |
| Total | 186 (100) | 186 (100) |
Table 3: Distribution of the various respiratory conditions with or without co morbidities
From Table 4, a comparison of the CDC determined cases (see Definitions) with the hospital diagnosed ones showed that of the 78 children who were diagnosed to have bronchopneumonia, 16 did not meet the CDC applied. However, for reactive airway disease, the initial figure of 30 increased by 13 when all the selected cases were subjected to CDC. The CDC rejected 6 of the 17 cases that were diagnosed as bronchiolitis. Further comparative analysis of the cases identified with the CDC with the hospital diagnoses showed that nine of the 22 children who were wrongly diagnosed to have bronchopneumonia had reactive airway disease; one had bronchiolitis while 12 had other respiratory diagnoses or co-morbid conditions. Likewise, two of the 30 children who were diagnosed to have reactive airway disease actually had bronchopneumonia and bronchiolitis respectively. A total of five out of 17 children who were diagnosed to have bronchiolitis actually had reactive airway disease by CDC.
| Case Definition Criteria | ||||
|---|---|---|---|---|
| Hospital Diagnosis | Other respiratory diseases/Co-morbidities | BP | RAD | BL |
| n (%) | n (%) | n (%) | n (%) | |
| Other respiratory diseases/Co-morbidities | 44 (62.9) | 5 (8.1) | 12 (27.9) | 0 (0.0) |
| BP | 12 (17.1) | 56 (90.3) | 9 (20.9) | 1 (9.1) |
| RAD | 11 (15.7) | 1 (1.6) | 17 (39.5) | 1 (9.1) |
| BL | 3 (4.3) | 0 (0.0) | 5 (11.6) | 9 (81.8) |
χ2 = 181.387, P < 0.001
Table 4: Diagnoses based on case definition criteria compared with hospital diagnoses
Table 5 shows that 56 out of 78 children with bronchopneumonia were correctly diagnosed (true positives); sensitivity-90% while 102 out of 124 infants without bronchopneumonia were correctly diagnosed (True negatives); specificity- 82%. The positive and negative predictive values indicate that a child diagnosed with bronchopneumonia by a doctor, has 72% chance of actually having bronchopneumonia while a child who was said not to have bronchopneumonia by a doctor, has 94% chance of not actually having bronchopneumonia.
| Case Definition | Sensitivity | Specificity | PPV | NPV | ||
|---|---|---|---|---|---|---|
| BP | None | |||||
| BP | 56 | 22 | 90% | 82% | 72% | 94% |
| None | 6 | 102 | - | - | - | - |
| RAD | None | - | - | - | - | |
| RAD | 17 | 13 | 40% | 91% | 57% | 83% |
| None | 26 | 129 | - | - | - | - |
| BL | None | - | - | - | - | |
| BL | 9 | 8 | 82% | 95% | 53% | 99% |
| None | 2 | 167 | - | - | - | - |
Table 5: Sensitivity, Specificity and Predictive value for the three major respiratory conditions
Also, 17 out of 30 children with reactive airway disease were correctly diagnosed (true positives) with a sensitivity of 40% and 129 out of 142 children without reactive airway disease diagnosed correctly (True negatives); specificity-91%. The positive predictive value shows that a child diagnosed to have reactive airway disease by a doctor, has 57% chance of actually having reactive airway disease. The negative predictive value shows that a child diagnosed as not to have reactive airway disease by a doctor, has 83% chance of not actually having reactive airway disease.
Of the 17 children who were diagnosed as having bronchiolitis, 9 were correctly diagnosed (True positives) with a sensitivity of 82%; and 167 out of 175 children without bronchiolitis were diagnosed correctly as not having the disease (True negatives); specificity-95%. The positive predictive value shows that a child diagnosed to have bronchiolitis by a doctor, has 53% chance of actually having bronchiolitis. The negative predictive value shows that a child diagnosed without bronchiolitis by a doctor, has 99% chance of not actually having bronchiolitis.
Discussion
Pneumonia remains a common source of morbidity in children while reactive airway disease and bronchiolitis are the other common conditions encountered in a pediatric emergency department (ED) [1]. Considering the diseases at presentation, bronchopneumonia accounted for 41.9%, of the cases admitted; while reactive airway disease and bronchiolitis accounted for 16.1% and 9.1% respectively. Using the case definition criteria, the prevalence of bronchopneumonia became lower by 8.6%, while reactive airway disease increased by 7%. Bronchiolitis decreased by 3.2%. This finding of these three conditions as the commoner acute respiratory conditions in children is similar to the findings by other workers [1,3,11]. Bronchopneumonia and bronchiolitis were identified as the major causes of communicable respiratory illnesses while asthma was one of the topmost causes of noncommunicable diseases admitted in a study that analyzed the pattern of respiratory diseases in a developing country [2]. While this study did not show a significant sex difference in presentations of the three conditions, there was however a significant difference in the median age of presentation, reactive airway disease having a toddler age presentation while bronchopneumonia is second half of infancy and bronchiolitis, first half of infancy.
The prevalence of pneumonia in studies that excluded children with a known history of asthma varied widely, ranging from 8.6% to 35% [2-4]. Prevalence of pneumonia in studies conducted among children with wheezing also varied widely, from 1% to 23% [9-12]. However, several of those studies were limited by their exclusion of children >2 years of age, as well as children with a history of wheezing [10-12]. About 23.1% of cases in this index study could not be determined when the CDC was applied. These were mainly because of entries by the attending physicians which were not complete to be useful and also possibly due to CDC which concentrated on features on admission and missed out previous episodes and family history information which could have diagnostic usefulness in diseases in this study grouped under reactive airway disease.
With increasing control of infectious respiratory diseases, efforts have shifted to non-communicable diseases like asthma which accounts for over 30% of all pediatric hospitalizations in the United States [4]. Although asthma causes 180,000 deaths worldwide each year, its greatest burden is the morbidity and disruption of lives that it causes [5].
The results of the present study reveal that when CDC were applied to the initial hospital diagnosis of bronchopneumonia and bronchiolitis, the prevalence rates dropped while the number of cases of reactive airway disease increased. This is not surprising because these are 3 conditions with similar symptoms though they are distinct diseases that require different treatment approaches. Reactive airway disease exacerbations may have clinical presentation like pneumonia in young children. Additionally, reactive airway disease and bronchiolitis are closely related in aetio-pathogenesis and clinical presentation [6]. The fact that these similarities present a challenge to the attending doctor is shown by the positive and negative predictive values of the attending doctors in this study. While the doctors can be said to correctly diagnose bronchopneumonia in 72% of cases, they however were capable in 94% of cases to correctly say a patient didn’t have bronchopneumonia. In the case of reactive airway disease and bronchiolitis, 57% and 83% and 53% and 99% respectively were the positive and negative predictive values. Clearly, diagnosing all these 3 conditions have been less than optimal even in the hands of clinicians but more so for reactive airway disease and bronchiolitis. The reason for this may not be far-fetched since so much awareness is being created about pneumonias in children and this cannot be without consequences. These values particularly for reactive airway disease may also have been affected by not considering the previous histories and family histories in our CDC.
The change in prevalence rates after applying the CDC and these predictive values suggest that there may be misrepresentation of the burden of these diseases with overdiagnosis of pneumonia and under-diagnosis of reactive airway disease. Nantanda et al. [11] in Uganda noted that the findings of their study support current arguments that, using WHO guidelines, bacterial pneumonia is overdiagnosed.
Over-diagnosis of pneumonia and under-diagnosis of asthma may be contributing to significant untreated respiratory morbidity and mortality among children less than five years in low-income countries [6]. Recognition of this trend and its correction may improve the quality of care given to these children.
Bearing in mind that these are 3 distinct diseases that require different treatment approaches, it will be important therefore to attempt to make the right diagnoses and for the appropriate treatment to be given. For instance, antibiotics would often be used irrationally due to misdiagnosis of reactive airway disease as bronchopneumonia. This can contribute to drug resistance, while increasing morbidity and cost of care. So also is a possible apparent worsening of severity of the respiratory condition if considered as bronchopneumonia and not rightly reactive airway disease or bronchiolitis.
As is often observed in retrospective studies, entries in patients’ folders were a challenge in this study. Secondly, the CDC, particularly as pertaining to reactive airway disease may not have been as sensitive and specific as would have been necessary. Notwithstanding these however, it can be said from the data here that there is a real need for a prospective study to determine these prevalence using refined CDC.
Conclusion
There is need for a review of the criteria for diagnosis of these respiratory conditions in children that are similar to forestall the danger of misdiagnosis and inappropriate treatment of children with these conditions.
References
- Akanbi MO, Ukoli CO, Erhabor GE, et al. The burden of respiratory disease in Nigeria. Afri J Resp Med 2009; 4: 10-17.
- Ferkol T, Schraufnagel D. The Global Burden of Respiratory Disease. Ann Am Thorac Soc 2014; 11: 404-406.
- Oguonu T, Ayuk AC, EdeluBO, et al. Pattern of respiratory diseases in children presenting to the paediatric emergency unit of the University of Nigeria Teaching Hospital, Enugu: A case series report. BMC Pulmonary Medicine 2014; 14: 101.
- http://data.unicef.org/child health/pneumonia.html
- Falade AG, Tschappelar H, Greenwood BM, et al. Use of simple clinical signs to predict Pneumonia in young Gambian children: the influence of malnutrition. Bull World Health Organ 1995; 73: 299-304.
- World Health Organization. Integrated Management of Childhood Illness (IMCI) (revised). Geneva, World Health Organization/The United Nation Children’s Fund (UNICEF), 2014.
- World Health Organisation Pocket Book of Hospital Care for Children: Guidelines for the management of common childhood illnesses. Second edn. 2013.
- Al-Dabbagh SA, Al-Zubaidi SN. The validity of clinical criteria in predicting pneumonia among children under five years of age. Iraq Journal of Family & Community Medicine 2004; 11: 11-16.
- Bradley JS, Byington CL, Shah SS, et al. The management of community-acquired pneumonia in infants and children older than 3 months of age: Clinical practice guidelines by Pediatric Infectious Diseases Society and Infectious Diseases Society of America. Clinical Infectious Diseases: An official publication of the Infectious Diseases Society of America 2011; 53: e25-76.
- Lanata CF, Rudan I, Boschi–Pinto C, et al. Methodological and quality issues in epidemiological studies of acute lower respiratory infections in children in developing countries. Int J Epidemiol 2004; 33: 1362-1372.
- Nantanda R, Tumwine JK, Ndeezi G, et al. Asthma and pneumonia among children less than five years with acute respiratory symptoms in Mulago hospital, Uganda: Evidence of under-diagnosis of asthma. Plos One 2013; 8: e81562.
- Bassat Q, MachevoS, O’Callaghan-Gordo C, et al. Distinguishing malaria from severe pneumonia among hospitalized children who fulfilled integrated management of childhood illness criteria for both diseases: A hospital-based study in Mozambique. Am J Trop Med Hyg 2011; 85: 626-634.
- Ostergaard MS, Nantanda R, Tumwine JK, et al. Childhood asthma in low income countries: An invisible killer? Prim Care Respir J 2012; 21: 214-219.