Current Pediatric Research
International Journal of Pediatrics
Mayer-Rokitansky-Kuster-Hauser Syndrome: Typical and atypical MRI findings
Mohamed Muyaser* Naif Rasha Nadeem Ahmed, Abeer Wali Ahmed
Department of Surgery, College of Medicine, Ninevah University, Mosul, Iraq
- Corresponding Author:
- Mohamed Muyaser
Department of Surgery
Ninevah
Mosul
Iraq
Tel: +964 771-291-3336
E-mail: drnihadkhalawe@gmail.com
Accepted date: 15th November, 2021
Background: The Mayer-Rokitansky-Kuster-Hauser Syndrome (MRKHS) is a reproductive tract congenital malformation, characterized by the absence or hypo plastic uterus and upper two thirds of the vagina in an otherwise normal female. Aims: This study is to analyze the MRI findings in group of MRKHS patients of both typical and atypical type. Methods: A cross sectional study, held in Mosul city, over a period of a year from October 2020 to October 2021, Female patients who was having MRI (Magnetic Resonance Imaging), done to them as a part of radio diagnosis workup of primary amenorrhea, were included in the study 1.5 tesla MRI scanner was used. Results: The studied patients are 23 females, age range (16 years-23 years), average 17.4 years, Std. Deviation 2.03 years. MRKHS type I is noted in (16/23) patients (69.5%) and MRKHS type II in (7/23) patients (30.4%), no MURCS subtype was identified. All the patients (100%) have absent uterus, cervix and upper vagina; small uterine buds are preserved in 17 patients (73.9%). Distended uterine buds with ipsilateral tubal dilatation is noted in 6 cases (26%) (Unilateral in 13% and bilateral in 13%). The lower vagina and external genetalia are not affected by the anomalies, however the lower vagina are very small (less than 1cm), in 4 cases (17%). The ovaries and the fallopian tubes appear to be unaffected by the malformation in 18 cases (78.2%), the extragenital associated findings were include renal anomalies in 3 cases (13%), in a form of ectopic kidney and renal agenesis, simple ovarian cysts were evident in 6 cases (26%), no detectable skeletal congenital abnormalities. Conclusion: MRI plays an important role in the evaluation of primary amenorrhea; it can detect congenital abnormalities of mullarian duct as those caused by MRKHS. It also can help in the diagnosis of extragenital renal or skeletal abnormalities, thus MRI exam should include the abdomen as well.
Keywords
Mayer-Rokitansky-Kuster-Hauser Syndrome, Primary amenorrhea, Mullarian agenesis, Uterine agenesis.
Introduction
The Mayer-Rokitansky-Küster-Hauser Syndrome (MRKHS), is one of the female reproductive tract congenital malformations, characterized by the absence or hypo plastic uterus and upper two-thirds of the vagina in otherwise normal 46, XX karyotype. The ovaries and external genitalia are usually not affected [1,2]. MRKHS is the second most common cause of primary amenorrhea in females [3]. It is found in 1/4500-5000 women [4-6]. The name Mayer–Küster–Rokitansky was first given to this syndrome by Hauser and scheiner in 1961 the other name of MRKHS is Mullerian agenesis [1,5]. The human reproductive system arises from the Mullerian and Wolffian ducts in an undifferentiated embryo, female genetic sex will trigger differentiations of ovaries, consequently. Mullerian duct will develop into uterus, cervix, upper vagina as well fallopian tubes thus any disturbance during period of development will result in Mullerian ducts malformation [7].
According to The European Society of Human Reproduction and Embryology and the European Society for Gynecological Endoscopy (ESHRE/ESGE, CONUTA working group), The uterine congenital malformation were categorized into five classes, The MRKHS is one of the most severe forms of malformation (Class 5) (U5) [8]. The MRKHS etiology is still unclear, it is mainly sporadic, however increasing the number of the recorded familial cases may suggest that at least a subgroup of MRKHS may be hereditary; the syndrome appears to be inherited in an autosomal dominant pattern, with variable expression and incomplete penetrance or a multifactorial or polygenic etiology [9]. Recent researches in the genetic of MRKHS suspected a mutation in homeobox genes, mainly Hoxa which are located in an area that is responsible directly for the development of the uterus, cervix, and vagina [10-13].
Generally, the MRKHS is divided into two main subtypes, MRKHS type 1 or typical MRKHS, that is characterize by the presence of normal ovaries, tubes with normal renal system and no other associated anomalies and MRKHS type 2, or atypical which is characterized by abnormal ovaries, ovarian tubes, as well renal or spinal agenesis, the MURCS association is described in some patients of type II, it represents the most severe type, and characterized be mullerian, renal and cervicothoracic congenital malformation. Because of the psychological and reproductive impact that the diagnosis of MRKHS will carry on the affected patient’s life the diagnosis should be disclosed in a sensitive way [14]. The diagnosis of MRKHS usually starts with careful physical examination by a pediatricians or more commonly a gynecologists to the external genitalia, then checking of the secondary sexual characteristics which are usually normal Ultra Sound (US) examination by trans abdominal or trans perineal approach is held to reveal absence of the uterus and the cervix with the presence of normal ovaries, then the patients usually has MRI (Magnetic Resonance Imaging) examination done to her [15]. MRI is regarded as the gold standard for the diagnosis of MRKHS, It is a non-invasive exam, and has advantages over the CT (Computed Tomography) scan, where it lacks the risk of radiation, carries better delineation of Mullerian structures (whether it shows complete or partial agenesis), it can also show the endometrium in the uterine remnant if present. MRI as well shows the ovaries, ovarian and adnexal pathologies and extragenital malformations, with a good inter-rater agreement with laparoscopic examination [16,17]. The US and the MRI examination should be extended to include the urinary system where the renal malformation has a well-documented association with the syndrome. The laparoscopy is rarely needed and it’s indicated only to relieve severe abdominal pain caused by retained menstrual blood in the Müllerian remnant, when surgical removal of the remnant is intended [18]. Screening of the other congenital malformations as skeletal, cardiac, gastrointestinal is not a routine, unless is suggested by relevant patient’s complaints or relevant finding in physical exam [19,20].
Chromosomal analysis is usually done to the affected patients, MRKHS patients are usually characterized by a normal 46, XX karyotype. Laboratory examinations of gonadotropins hormones (LH, FSH) as well androgens and estradiol are usually found to be of normal values in MRKHS and hence not a routine. The aim of our study is to analyze the MRI findings in a group of MRKHS patients of typical and atypical type.
Materials and Methods
After the approval from the ethical committee of collage of medicine in Ninevah University, we conducted a cross sectional study , in Mosul city over a period of a year from October 2020 to October 2021, Female patients who were presented with primary amenorrhea and had a normal secondary sexual characteristics, normal female 46, XX karyotype and was having MRI (Magnetic Resonance Imaging), done to them as a part of radio diagnosis workup of primary amenorrhea, were studied, those with imaging findings of agenesis or dysgenesis of the reproductive tract (MRKHS),were included in the study, the exclusion criteria include unavailable or abnormal karyotype, or imaging finding other than mullerian duct agenesis, or patients who did not have MRI exam for any reason.
The studied patients were 23 in number, they were referred by gynecologists or less commonly by pediatricians, The diagnosis of MRKHS was depending on the physical examinations, radiological examinations in a form of US and MRI, some other lab exams or radio imaging exam were done as indicated in each case, the data were collected by analyzing Imaging findings mainly ultrasound and MRI of the abdomen and pelvis on the background of clinical information. Informed Patient consent was obtained from the all patients. The initial Ultrasound examination was done by using the HS40 ultrasound machines (Samsung company made in Korea) a Trans abdominal approach through a convex probe: CA2-8AD.CF4-9. The patient was instructed to have adequate urinary bladder filling, for better evaluation of the reproductive tract.
The MRI examination was done by using 1.5 T Philips Achieve MRI scanners and a standard 16-channel phased array pelvis and abdomen coil. With the following parameters:
•T1- Weighted images TR 501 ms; TE 20 ms; Matrix-276 × 280; Section thickness 3 mm; FOV 28.8 cm,
•T1W (SPIR): TR 612 ms; TE 10 ms, Matrix 200 × 170; Section thickness 5 mm, FOV 26 cm.
•T2-weighted (axial): TR 4709 ms; TE 100 ms; Matrix 248 × 209; Section thickness 4 mm; FOV 30 cm;
•T2W (sagittal): TR 3000 ms; TE: 90 ms; Matrix 172 × 140; Section thickness 5 mm; FOV 23.9 cm;
•STIR (coronal): TR 2990 ms; TE 80 ms; Matrix 184 × 170; Section thickness 4 mm; FOV 26.7 cm;
•STIR (axial): TR 5980 ms; TE 80 ms; Matrix 18 × 160; Section thickness 4 mm; FOV 26 cm.
•Statistics: The Microsoft excel Version16.0.12430.20120; were used to save the Data; the Date then analyzed by using Statistical Package for Social Sciences IBM (SPSS) 22; For continuous variables as age; measures of central tendency and dispersion were used. The categorical variables were expressed in frequency and percent.
Results
Table 1 shows the studied patients are 23 females; their ages range between 16 years-23 years; with an average age of 17.4 years; Std. Deviation 2.03 years. The studied twenty-three females are classified as having MRKHS type 1 (16/23) 69.5%; and MRKHS type II (7/23) 30.4%; No MURCS subtype cases were identified.
| Symptoms | No | percent |
|---|---|---|
| primary amenorrhea | 23 | 100.00% |
| cyclic abdominal pain | 6 | 26.00% |
| Types | ||
| MRKH type I | 16 | 69.50% |
| MRKH type II | 7 | 30.40% |
| Family history | ||
| Present | 0 | 0.00% |
| Absent | 23 | 100.00% |
| Genital malformation | ||
| 1/uterus | ||
| Present | 0 | 0.00% |
| Absent | 23 | 100.00% |
| uterine buds present and small | 17 | 73.90% |
| uterine buds are present with | 6 | 26.00% |
| unilateral or bilateral distension | ||
| 2/Cervix and upper vagina | ||
| Present | 0 | 0.00% |
| Absent | 23 | 100.00% |
| 3/Lower Vagina | ||
| Present | 23 | 100.00% |
| Absent | 0 | 0.00% |
| present but very small | 4 | 17.30% |
| 4/ovaries and Tubes | ||
| Both ovaries are Present | 18 | 78.20% |
| absent right ovary and its ipsilateral tube | 1 | 4.30% |
| absent left ovary and its ipsilateral tube | 4 | 17.30% |
| maldsescent both ovaries | 1 | 4.35 |
| Associated malformation | ||
| Congenital renal malformation | 3 | 1.30% |
| Others | 0 | 0.00% |
Table 1. Frequency and percent of symptoms: Family history and various genital and extra genital malformations.
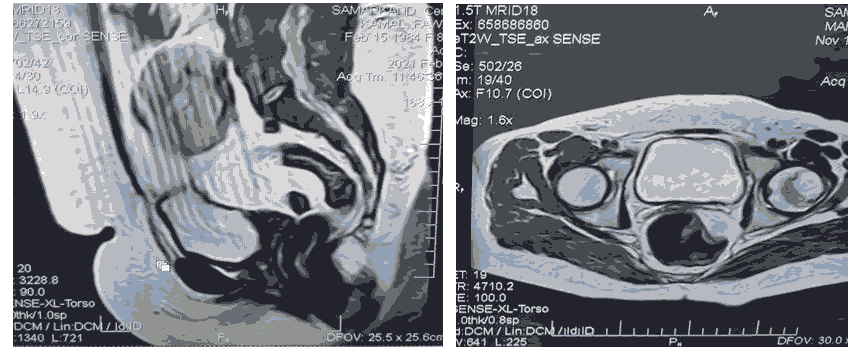
All the studies females presented with primary amenorrhea and positive secondary sexual characteristics; with 6 of the patients presented as well with cyclic abdominal pain. All the patients have absent uterus; cervix and upper vagina (Figure 1). The cranial part of the reproductive tract represented by the presence of small uterine buds is preserved in 17 patients (73.9%). Some of the uterine buds (Mullerian duct remnant) are seen dilated with blood (containing functional endometrium); and associated with ipsilateral tubal dilatation (hydrosalpinx) this seen in 6 patients (26%); unilaterally (one of the buds is dilated with unilateral hydrosalpinx) in three cases of them and bilaterally (distended both buds and bilateral hydrosalpinx) in the other three cases. The lower vagina and external genetalia are not affected by the anomalies; however the lower vagina are very small (less than 1 cm) in 4 cases (17%).
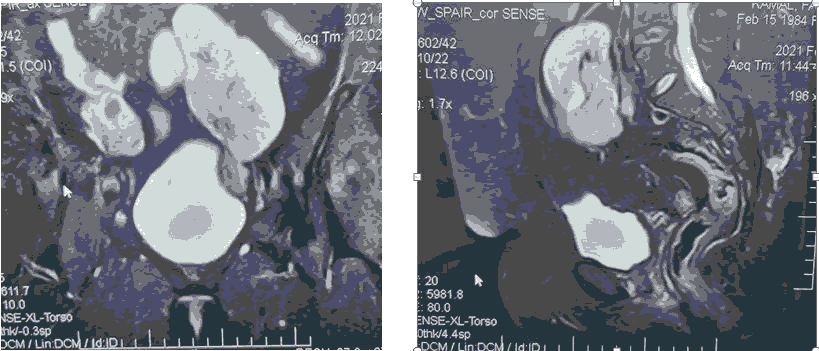
The ovaries and the fallopian tubes appear to be unaffected by the malformation in 18 cases (78%); in 5 cases (21%) however; unilateral absence of the ovary and ipsilateral tube is evident (Right=1; Left=4); one of the cases show bilateral maldescended ovaries. The MRI examination in the current study was including the abdomen in addition to the pelvis; the exam revealed multiple detected associated findings; they include associated congenital renal anomalies in 3 cases (13%); in a form of ectopic pelvic kidney (Figure 2). Renal agenesis with contralateral ectopic kidney; as well unilateral renal agenesis; no bony or cardiac malformation can be noted; among the other radiological findings are the presence of simple ovarian cysts in 6 cases (26%); with equal frequency in each ovary; no detectable skeletal congenital abnormalities; no symptoms or physical findings; mandating patients screening for other abnormality like cardiac; skeletal or auditory malformation. Family history of congenital malformation of reproductive tract couldn’t be identified in any of the included cases; however in a single case; the family history of unilateral renal agenesis was evident.
A B
A. T2WI sagittal plain
B. T2WI axial plain
A B
A. STIR coronal plain
B. STIR sagittal plain
Discussion
MRKHS is an uncommon however not rare congenital malformation. Female with MRKHS cannot usually menstruate; engage in penile vaginal intercourse; cannot get pregnancy without surgical and assisted reproductive techniques and she has also the possibility to have an associated renal; skeletal and cardiac anomalies; all these will have a great psychological and physical impact in the affected individual; reflected in her life quality and social relations; better understanding of the syndrome may aid in the diagnosis and the management [14].
In our study the average age of the presentation is 17.3 years; which nearly the same is as found by a nationwide registry-based study held in Denmark on the prevalence of MRKHS by Herlin et al. In which the average age was found to be (17.5 years). The main presenting symptoms in our study is the primary amenorrhea (100% of the cases); same was found by Herlin et al; in the mentioned study the primary amenorrhea was the presenting symptoms in 85%. In our study the second most common presenting symptom is the cyclic abdominal pain (26%); the cyclic abdominal pain and the dyspareunia represented the second and the third most common presenting symptoms (4.5% and 3.5% respectively) in Herlin et al. no reported dyspareunia in our study; as our sample is composed totally of virgin females ; Although MRKHS is thought to be sporadic in etiology; an increasing number of familial cases; had led to the conclusion that inheritance may play a role in the syndrome etiology. In the present study our cases are all assumed to be sporadic; no family history of genital anomalies were detected; lack of familial cases were also seen in some other studies; including Deng et al.
There are mainly two types of MRKHS according to the associated anomalies previous literatures including studies done in large samples in Europe as Greatsas et al. and Herlin et al. as well large studies done in china as Pan HX and Luo et al. and Deng et al. had shown that the most common type is type I followed by type II; in the present study; the same is found as the commonest type is type I (typical MRKHS ) (69.5%); followed by type II (atypical MRKHS)(30.4%) [21-23]. The typical MRKHS cases in the present study are classified according to The VCUAM classification (Vagina Cervix Uterus Adnex Associated Malformation) classification; a classification system which is developed by Opplet et al. for better understanding of female genital malformations as V5b; C2b; U4b; A0; M0; the same finding was reported by Pan et al. in which the same VCUAM class is also reported in most of (92.8%) of the MRKHS cases [24].
The atypical finding like associated renal anomalies is noted in 1.3% in the present study; which is markedly lower than that noted by some other Chinese studies as in Deng S et al. (13.2%) and in Pan et al. (5.1%) and much more lower than that recorded in European studies like Herlin et al. and Opplet et al. Rall et al. and Greatsas et al. were the percent was 26.6%-44.5% [25]. No skeletal abnormalities are noted in the current study sample; while the skeletal abnormalities were recorded with a wide range of variability in its prevalence (1.7%-40%) in the previous studies [26]. The cardiac anomalies which is reported infrequently with MRKHS (no or few cases up to 3.6%); none of the cardiac abnormality were reported in the present study however. To our knowledge no published study in the imaging findings of MRKHS in our locality; however the main limitation of the current study is the small patient’s number as well as loosing contact with some patients in order to have the complete clinical picture leading them to be excluded from the study.
Conclusion
MRI examination plays an important role in the evaluation of females with primary amenorrhea it can detect congenital abnormalities of Mullarian duct caused by MRKHS and help in differentiating it to its types through showing other extragenital malformations like renal or spinal abnormalities and thus the MRI exam should not only include pelvic organs but extended to include the abdomen as well.
Abbreviations
CT: Computed Tomography; MRCUS: Mullerian duct aplasia; Renal aplasia; and Cervicothoracic Somite dysplasia; MRI: Magnetic Resonance Imaging; MRKHS: Mayer-Rokitansky-Küster-Hauser Syndrome; Std. Deviation: Standard Deviation; STIR: Short Tau Inversion Recovery; T1W: T1 Weighted Image; T2W: T2 Weighted Image; US: Ultra Sound; VCUAM Classification: Vagina Cervix Uterus Adnex Associated Malformation Classification.
References
- Hauser GA, Schreiner WE. Mayer-Rokitansky-Kuester syndrome. Rudimentary solid bipartite uterus with solid vagina. Schweiz Med Wochenschr 1961; 91: 381–384.
- Liszewska Kaplon M, Strozik M, Kotarski L, et al. Mayer-Rokitansky-Kuster-Hauser syndrome as an interdisciplinary problem. Adv Clin Exp Med 2020; 29(4): 505-511.
- Oppelt PG, Lermann J, Strick R et al. Malformations in a cohort of 284 women with Mayer-Rokitansky-Kuster-Hauser syndrome (MRKH). Reprod Biol Endocrinol 2012; 10: 51-57.
- Griffin JE, Edwards C, Madden JD. Congenital absence of the vagina: The Mayer-Rokitansky-Kuster-Hauser syndrome. Ann Intern Med 1976; 85(2): 224-236.
- Folch M, Pigem I, Konje JC. Mullerian agenesis: etiology, diagnosis, and management. Obstet Gynecol Surv 2000; 55(10): 644-649.
- Herlin M, Bjorn AM, Rasmussen M, et al. Prevalence and patient characteristics of Mayer–Rokitansky–Kuster–Hauser syndrome: a nationwide registry-based study. Hum Reprod 2016; 31(10): 2384-2390.
- Rahilly RO. The timing and sequence of events in the development of the human reproductive system during the embryonic period proper. Anat Embryol 1983; 166(2): 247-261.
- Grimbizis GF, Gordts S, Di SpiezioSardo A ,et al. The ESHRE-ESGE consensus on the classification of female genital tract congenital anomalies. Gynecol Surg 2013; 10(3): 199–212.
- Herlin M, Hojland AT, Petersen MB. Familial occurrence of Mayer–Rokitansky–Kuster–Hauser syndrome: A case report and review of the literature. Am J Med Genet A 2014; 164(9): 2276-86.
- Stribbe EH, Cremers CW, Willemsen WN, et al. The Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome without and with associated features: Two separate entities?. Clin Dysmorphol 1994; 3(3): 192–199.
- Duncan PA, Shapiro LR, Stangel JJ, et al. The MURCS association: Mullerian duct aplasia, renal aplasia, and cervicothoracic somite dysplasia. J Pediatr 1979; 95(3): 399-402.
- Oppelt P, Renner SP, Kellermann A, et al. Clinical aspects of Mayer–Rokitansky–Kuester–Hauser syndrome: recommendations for clinical diagnosis and staging. Hum Reprod 2006; 21(3): 792-797.
- Fontana L, Gentilin B, Fedele L, et al. Genetics of Mayer–Rokitansky–Küster–Hauser (MRKH) syndrome. Clin Genet 2017; 91(2): 233-246.
- Bean EJ, Mazur T, Robinson AD. Mayer-Rokitansky-Küster-Hauser syndrome: sexuality, psychological effects and quality of life. J Pediatr Adolesc Gynecol 2009; 22(6): 339-346.
- Herlin MK, Petersen MB, Brannström M. Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome: A comprehensive update. Orphanet J Rare Dis 2020; 15(1): 1-6.
- Lermann J, Mueller A, Wiesinger E, et al. Comparison of different diagnostic procedures for the staging of malformations associated with Mayer-Rokitansky-Kuster-Hauser syndrome. Fertil Steril 2011; 96(1) :156–159.
- Preibsch H, Rall K, Wietek BM, et al. Clinical value of magnetic resonance imaging in patients with Mayer Rokitansky-Kuster-Hauser (MRKH) syndrome: Diagnosis of associated malformations, uterine rudiments and intrauterine endometrium. Eur Radiol 2014; 24: 1621–1627.
- ACOG Committee Opinion No. 728: Mullerian Agenesis: Diagnosis, Management, and Treatment. Obstet Gynecol. 2018; 131: 35–42.
- Morcel K, Guerrier D, Watrin T, et al. The Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome: Clinical description and genetics. J Pediatr Adolesc Gynecol 2008; 37(6): 539-546.
- Deng S, He Y, Chen N, et al. Spectrum of type I and type II syndromes and associated malformations in Chinese patients with Mayer-Rokitansky-Küster-Hauser syndrome: A retrospective analysis of 274 cases. J Pediatr Adolesc Gynecol 2019; 32(3): 284-287.
- Strübbe EH, Thijn CJ, Willemsen WN, et al. Evaluation of radiographic abnormalities of the hand in patients with the Mayer-Rokitansky-Küster-Hauser syndrome. Skeletal radiol 1987; 16(3): 227-231.
- Creatsas G, Deligeoroglou E, Christopoulos P. Creation of a neovagina after Creatsas modification of Williams vaginoplasty for the treatment of 200 patients with Mayer-Rokitansky-Kuster-Hauser syndrome. Fertil Steril 2010; 94(5): 1848-1852.
- Pan HX, Luo GN. Phenotypic and clinical aspects of Mayer-Rokitansky-Küster-Hauser syndrome in a Chinese population: An analysis of 594 patients. Fertil Steril 2016; 106(5): 1190-1194.
- Oppelt P, Renner SP, Brucker S, et al. The VCUAM (Vagina Cervix Uterus Adnex–Associated Malformation) classification: A new classification for genital malformations. Fertil Steril 2005; 84(5): 1493-1497.
- Rall K, Eisenbeis S, Henninger V, et al. Typical and atypical associated findings in a group of 346 patients with Mayer-Rokitansky-Kuester-Hauser syndrome. J Pediatr Adolesc Gynecol 2015; 28(5): 362-368.
- Oppelt PG, Lermann J, Strick R, et al. Malformations in a cohort of 284 women with Mayer-Rokitansky-Küster-Hauser syndrome (MRKH). Reprod Biol Endocrinol 2012; 10(1): 1-7.