Current Pediatric Research
International Journal of Pediatrics
Hospitalization cost in infants with hypoglycemia.
Brook T Alemu1*, Hind A Beydoun2, Matthew Hoch3, Bonnie Van Lunen4, Muge Akpinar-Elci4
1Western Carolina University, School of Health Sciences, Cullowhee, NC, USA
2Johns Hopkins University School of Medicine, Baltimore, MD, USA
3University of Kentucky, College of Health Sciences, Lexington, KY, USA
4Old Dominion University, College of Health Sciences, Norfolk, VA, USA
- Corresponding Author:
- Brook T. Alemu, PhD, MPH
School of Health Sciences, Western Carolina University
3971 Little Savannah Rd, Cullowhee, NC 28723, USA
Tel: 828-277-2647
Fax: 828-277-7446
E-mail: balemu@wcu.edu
Accepted date: December 05, 2018
This study sought to determine the overall hospital cost estimates in neonates with hypoglycemia, compare hospital cost in premature and non-premature neonates, and identify predictors of increased hospital cost. The median (interquartile range) cost estimate in premature and non-premature neonates were $12,755 ($4,550-$30,339) and $2,360 ($1,153-$3,736), respectively. Increased cost was observed, when more than five procedures was performed during the same hospitalization (OR 10.13, 95% CI 8.67-11.83, p<0.0001), when hospital bed size medium (OR 1.37, 95% CI 1.16-1.61, p=0.0002) or ≥ 400 (OR 1.65, 95% CI 1.41-1.92, p<0.0001), when hospital length of stay exceeded 15 days (OR 44.97, 95% CI 41.49-48.73, p<0.0001), in teaching hospitals (OR 1.97, 95% CI 1.82-2.13, p<0.0001), in of the presence of chronic conditions (OR 2.46, 95% CI 2.27-2.66, p<0.0001), comorbidities (OR 2.11, 95% CI 1.90-2.35, p<0.0001), prematurity (OR 2.39, 95% CI 2.20-2.60, p<0.0001), and death (OR 2.95, 95% CI 2.13-4.09, p<0.0001). Neonates with hypoglycemia consumed 11% of resources associated with hospital births while accounting for only 1.5% of hospitalization. This study identified factors associated with increased cost in neonatal hypoglycemia.
Keywords
Birth complication, Hospital cost, Hypoglycemia, Neonates, Prematurity.
Introduction
Neonatal Hypoglycemia (NH) is a common metabolic abnormality in newborns due to inability to maintain glucose homeostasis [1,2]. Throughout gestation, mothers provide all the glucose for their fetuses via facilitated diffusion across the placenta according to a maternal-to-fetal glucose concentration gradient [3]. The disruption of this process can lead to several acute and chronic illnesses. The most common symptoms of NH are shakiness, tachycardia, lethargy, and temperature irregularities [4]. In the presence of these symptoms, NH is defined as capillary plasma glucose of less than 46 mg/dl (2.6 mmol/l) [4,5]. Several clinical conditions could be associated with NH that could affect glucose homeostasis including asphyxia, congenital heart disease, decreased substrate availability as a result of birth defects, prematurity and fetal growth restriction, islet cell hyperplasia, and Beckwith-Wiedemann Syndrome [6-10]. Prolonged NH may also cause neuroglycopenic signs such as seizures, coma, cyanotic episodes, apnea, respiratory distress, and hypothermia [2].
Previous NH studies mainly focused on the clinical risk factors and analyses aimed at improving the management and care of this condition. However, the economic burden and overall hospital cost estimates of NH has not been studied at the national level in the United States (US). The economic burden of hypoglycemia has been adequately addressed in the adult population [11-16]. This study sought to determine the overall hospital cost estimates in neonates with hypoglycemia and compare hospital cost in premature and non-premature newborns. The study also sought to identify predictors of increased hospital cost.
Materials and Methods
This is a retrospective study based on the 2012 Kids’ Inpatient Database (KID) developed by the Healthcare Cost and Utilization Project (HCUP) of the Agency for Healthcare Research and Quality (AHRQ) [17]. The KID is the largest publicly available all-payer pediatric (≤ 20 years of age) inpatient care database in the United States. The database is a sample of pediatric discharges from all community, non-rehabilitation hospitals in 44 participating States. Systematic random sampling is used to select 10% of uncomplicated in-hospital births and 80% of other pediatric cases from each participating state. The 2012 KID database includes 4179 hospitals with 3,195,782 pediatric discharges. HCUP categorize hospital regions as northeast, midwest, south, and west. Hospital ownership, teaching status, location, bed size, and other important hospital characteristics were also included in the database. In total, 70 children’s hospitals (400,835 pediatric discharges) and 4,109 hospitals that admit all patients (2,794,947 pediatric discharges) were included in the 2012 database. As we are interested only in neonates, this analysis is limited to uncomplicated and complicated in-hospital births.
For the purpose of our analysis the inpatient core file, the hospital file, and cost-to-charge ratios file of the KID 2012 database were used. Neonates with hypoglycemia (775.6) were identified using the 9th version of the international classifications of diseases (ICD-9-CM). The outcome variable was identified by converting the total hospital charge to hospital cost estimates (Hospital Costs=Cost-to-Charge Ratios*Total Charges) [18-24]. Using the distribution of total hospital cost estimates we categorized hospital cost into increased hospital cost estimates (>75th percentile) and lower hospital cost estimates (≤ 75th percentile).
Neonatal comorbidities associated with hypoglycemia were defined as a dichotomous variable using ICD-9-CM codes (Appendix A). In this respect, the presence of any comorbidities associated with neonatal hypoglycemia such as jitteriness, hypotonia, lethargy, apnea, tachypnea, poor feeding, hypothermia, sepsis, seizures, neurodevelopmental deficits were used to create a dichotomous variable that indicates the morbidity status of newborns. In addition, demographic information (age, sex, and race), region of hospitals (Northeast, Midwest, South, West), hospitals teaching status, bed-size category (small, medium, large), admission date (weekend versus weekdays), length of hospital stay (LOS), number procedures performed during hospitalization (NPR), number of chronic conditions during hospitalization, expected primary payer, and in-hospital mortality was extracted for the purpose of the current analysis. Hospitalization for hypoglycemic neonates was categorized into premature and nonpremature using the Diagnosis Related Groups version 24 (DRG24) codes (386-388). DRG24 is assigned by the Centers for Medicare & Medicaid Services (CMS) DRG Grouper algorithm during HCUP processing and it been available since 2006 [17].
We used the Kolmogorov-Smirnov test (KS-Test) to assess normality for continuous variables. Groups were compared using the Wilcoxon-Mann-Whitney test for continuous variables and the χ2 test for categorical variables. For continuous variables data were presented in median and interquartile range (IQR). Whereas categorical variables were presented as numbers (n) and percentages (%). Odds ratios (OR) for increased hospital cost estimates were determined by using bivariate and multivariate logistic regression. All variables that were significantly associated with increased cost (p<0.05) were included in the multivariable logistic regression analysis. We used this stringent criterion for inclusion in the model was used because of the large sample size.
A p<0.05 was considered statistically significant for all tests. SAS® version 9.3 was used for the analysis (Institute Inc., Cary, NC, USA). In assessing the calibration of our model, we used the Receiver Operating Characteristics (ROC) curve to calculate c statistic and the Deviance– Pearson (D-P) goodness of fit statistics [18,19]. The two model evaluation measures carried out in this study should provide enough assurance regarding the accuracy of our model.
Results
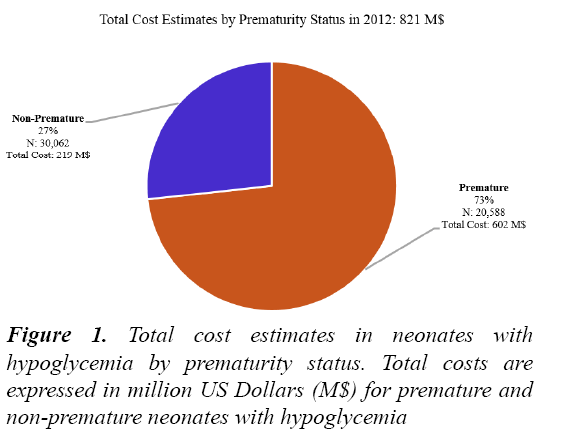
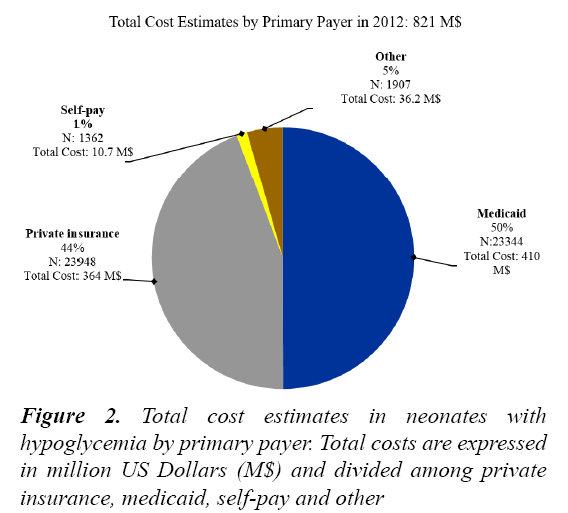
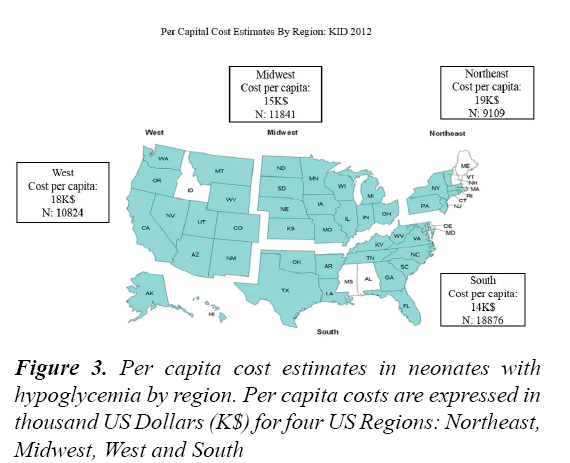
A total of 3,195,782 hospital discharges were included in the 2012 KID HCUP database, from which 1,107,573 were in-hospital births. From the total in-hospital birth we were able to identify 50,650 neonates with hypoglycemia (5%). In 2012, the total hospital cost in neonates with hypoglycemia was 821 M$. Since the total cost for inhospital births was 7692 M$, hospital cost in neonates with hypoglycemia represents 11%. Figure 1 indicates the relative proportion the cost that for premature (73%: 602 M$) and non-premature (27%: 219 M$) neonates. The median cost estimates in premature and non-premature neonates were $12,755 ($4,550-$30,339) and $2,360 ($1,153-$3,736), respectively. On the other hand, Figure 2 represents the distribution of hospital cost estimates by primary payers which are divided into Medicaid (50%: 410 M$), private insurance (44%: 364 M$), Self-pay (1%: 10.7 M$), and other (5%: 36.2 M$). In addition, Figure 3 indicates that the per capita cost estimates among the four U.S. regions, that are northeast (19 K$), Midwest (15 K$), South (14 K$), and West (18 K$). Total cost estimates that exceed the 75th percentile ($13,575) was defined as excessive cost associated with hospital discharge.
Table 1 represents characteristics of neonates with hypoglycemia that were categorized into two subgroups.
| Variables | Premature (N=20,588) (40%) |
Non-Premature (N=30,062) (60% ) |
Total (N=50,650) (100%) |
p-Value |
|---|---|---|---|---|
| Gender n (%) | ||||
| Male | 10,781(37.11) | 18,269 (62.89) | 29,050 (57.38) | <0.0001 |
| Female | 9,800 (45.42) | 11,778 (54.58) | 21,578 (42.62) | |
| Race n (%) | ||||
| White | 9,826 (38.88) | 15,448 (61.12) | 25,274 (55.40) | <0.0001 |
| Black | 3,599 (47.11) | 4,041 (52.89) | 7,640 (16.75) | |
| Hispanic | 2,893 (40.80) | 4,197 (59.20) | 7,090 (15.54) | |
| Asian/Pacific | 714 (38.02) | 1,164 (61.98) | 1,878 (4.12) | |
| Native Americans | 170 (38.99) | 266 (61.01) | 436 (0.96) | |
| Admission Day n (%) | ||||
| Weekday | 15,816 (39.51) | 24,216(60.49) | 40,032 (79.04) | <0.0001 |
| Weekend | 4,772 (44.94) | 5,846 (55.06) | 10,618 (20.96) | |
| Hospital n (%) | ||||
| Teaching | 12,952 (44.64) | 16,060 (55.36) | 29,012 (57.28) | <0.0001 |
| Non-Teaching | 7,636 (35.29) | 14,002 (64.71) | 21,638 (42.72) | |
| Bed Size n (%) | ||||
| Small (1-99) | 1,310 (30.83) | 2,939 (69.17) | 4,249 (8.39) | <0.0001 |
| Medium (100-399) | 5,071 (39.19) | 7,869 (60.81) | 12,940 (25.55) | |
| Large (≥ 400) | 1,4207 (42.46) | 19,254 (57.54) | 33,461 (66.06) | |
| Ownership n (%) | ||||
| Private | 15,161 (40.58) | 22,200 (59.42) | 37,361 (73.76) | <0.0001 |
| Public | 5,427 (40.84) | 7,862 (59.16) | 13,289 (26.24) | |
| Morbidity n (%) | 2,982 (49.01) | 3,102 (50.99) | 6,084 (12.01) | <0.0001 |
| Mortality n (%) | 0 (0) | 389 (100) | 389 (0.77) | |
| NPR#* | 2 (1-4) | 2 (0-2) | 4 (2-11) | <0.0001 |
| LOS days +* | 11 (2-24) | 3 (2-5) | 1 (0-3) | <0.0001 |
| +LOS, Hospital length of stay in days; #NPR, number of procedure. Data are presented in number (n) and percentage (%), or *Median and interquartile range (IQR) | ||||
Table 1: Characteristics of neonates with hypoglycemia by prematurity status
We observed that 40% (n=20, 588) of neonates were premature. Among infants included in the study, 55% were White, 17% Black, 16% Hispanic, 4% Asian/Pacific and 1% Native Americans while 57% and 43% of the neonates were male and female. The median values for premature and non-premature neonates were as follows: NPR 2 (IQR 1-4) and LOS 11 (5-24) and NPR 2 (IQR 0-2) and LOS 3 (2-5), respectively. In 2012, the prevalence of hypoglycemia among in-hospital births in the U.S. was 5% (n=50,650).
In the unadjusted analysis, all variables included in the models were independently associated with increased hospital costs (Table 2). The results from our multivariate analysis to determine factors associated with increased cost estimates among hypoglycemic neonates are presented in Table 3. Increased costs were observed, when more than five procedures were performed during the same hospitalization (OR 10.13, 95% CI 8.67-11.83, p<0.0001), when hospital bed size were between 100 and 300 (OR 1.37, 95% CI 1.16- 1.61, p=0.0002) and ≥ 400 (OR 1.65, 95% CI 1.41- 1.92, p<0.0001), when hospital length of stay exceeds 15 days (OR 44.97, 95% CI 41.49-48.73, P<0.0001), when hospitals have teaching status (OR 1.97, 95% CI 1.82-2.13, p<0.0001), in the case of chronic conditions (OR 2.46, 95% CI 2.27-2.66, p<0.0001), comorbidity (OR 2.11, 95% CI 1.90-2.35, p<0.0001), prematurity (OR 2.39, 95% CI 2.20-2.60, p<0.0001), and death (OR 2.95, 95% CI 2.13-4.09, p<0.0001).
| Variables | Unadjusted OR | B (SE) | 95% CI | p value |
|---|---|---|---|---|
| Female | 1.20 | 0.19 (0.02) | 1.16 1.26 | <0.0001 |
| Black | 1.65 | 0.50 (0.03) | 1.55-1.74 | <0.0001 |
| Hispanic | 1.37 | 0.31 (0.03) | 1.29-1.45 | <0.0001 |
| Asian/Pacific | 1.41 | 0.34 (0.05) | 1.27-1.56 | <0.0001 |
| Native Americans | 1.10 | 0.10 (0.11) | 0.88-1.38 | 0.3721 |
| Weekend | 1.14 | 0.14 (0.02) | 1.09-1.20 | <0.0001 |
| Medium (100-399) | 1.91 | 0.65 (0.05) | 1.74-2.10 | <0.0001 |
| Large (≥ 400) | 2.24 | 0.80 (0.05) | 2.05-2.45 | <0.0001 |
| Teaching Hospital | 2.28 | 0.83 (0.02) | 2.19-2.39 | <0.0001 |
| LOS+ >15 days | 95.36 | 4.56 (0.03) | 89.32-101.82 | <0.0001 |
| NPR# >5 | 43.21 | 3.77 (0.05) | 38.93- 47.96 | <0.0001 |
| Chronic Condition | 5.82 | 1.76 (0.02) | 5.57-6.08 | <0.0001 |
| Death | 6.01 | 1.79 (0.11) | 4.87-7.42 | <0.0001 |
| Premature | 8.95 | 2.19 (0.02) | 8.53-9.38 | <0.0001 |
| Morbidity | 3.45 | 1.24 (0.03) | 3.26-3.64 | <0.0001 |
| OR: Odds Ratio; B: Regression Coefficient; SE: Standard Error; CI: Confidence Interval; +LOS: Hospital Length of Stay in Days; #NPR: Number of Procedures | ||||
Table 2: Unadjusted ORs, 95% CIs, and p values from bivariate logistic regression analysis associated with increased cost estimates (>75th Percentile)
| Variables | Adjusted OR | B (SE) | 95% CI | p Value |
|---|---|---|---|---|
| Female | 1.01 | 0.01 (0.09) | 0.94-1.09 | 0.7439 |
| Black | 0.89 | -0.12 (0.05) | 0.8.0-0.98 | 0.0185 |
| Hispanic | 1.26 | 0.23 (0.05) | 1.13-1.39 | <0.0001 |
| Asian/Pacific | 1.95 | 0.67 (0.09) | 1.63-2.32 | <0.0001 |
| Native Americans | 1.57 | 0.45 (0.19) | 1.09-2.28 | 0.0163 |
| Weekend | 1.04 | 0.04 (0.05) | 0.95-1.14 | 0.3816 |
| Medium (100-399) | 1.37 | 0.31 (0.08) | 1.16-1.61 | 0.0002 |
| Large (≥ 400) | 1.65 | 0.50 (0.08) | 1.41-1.92 | <0.0001 |
| Teaching Hospital | 1.97 | 0.68 (0.04) | 1.82-2.13 | <0.0001 |
| LOS >15 days | 44.97 | 3.81 (0.04) | 41.49-48.73 | <0.0001 |
| NPR >5 | 10.13 | 2.32 (0.08) | 8.67-11.83 | <0.0001 |
| Chronic Condition | 2.46 | 0.90 (0.04) | 2.27-2.66 | <0.0001 |
| Death | 2.95 | 1.08 (0.17) | 2.13-4.09 | <0.0001 |
| Premature | 2.39 | 0.87 (0.04) | 2.20-2.60 | <0.0001 |
| Morbidity | 2.11 | 0.75 (0.05) | 1.90-2.35 | <0.0001 |
| OR: Odds Ratio; B: Regression Coefficient; SE: Standard Error; CI: Confidence Interval;+LOS: Hospital Length of Stay in Days; #NPR: Number of Procedures | ||||
Table 3: Adjusted ORs, 95% CIs, and p values from multivariate logistic regression analysis associated with increased cost estimates (>75th Percentile)
The area under the ROC curve (0.95, 95% CI 0.948- 0.953) indicated the predictive accuracy of the multivariate model. In addition, the results from the D-P goodness of fit (d=3820, df=3722) also expressed that the values for deviance (d) are not much larger than their degrees of freedom, suggesting that the fitted model cannot be rejected and leads to the conclusion that the model fits well [18].
Discussion
Our analysis of the 2012 HCUP KID database shows that hospital cost estimates in neonates with hypoglycemia consumed 11% of the resources associated with hospital births. We determined a 5% prevalence of NH among in-hospital births in the U.S during the year 2012. We also determined that medium and large hospital bed sizes, LOS, NPR, teaching hospitals, composite neonatal comorbidities, prematurity, occurrence of chronic conditions, and mortality were independently associated with increased hospital cost estimates in neonates with hypoglycemia.
Previous studies have focused on estimations of the economic cost of hypoglycemia in the adult population [11- 16]. To our best knowledge, this is the first study providing an empirical estimate of the hospital cost of neonatal hypoglycemia at the national level. It is worth noting that 100% of mortality and higher morbidity (51%) occurred in the non-premature group. As premature neonates are usually treated in neonatal intensive care units that provide around-the-clock care, non-premature babies appear to be prone to mortality and various hypoglycemia related comorbidities. This result is consistent with previous studies [20-22] in that neonates with asymptomatic hypoglycemia may easily be neglected of proper care which may lead to acute comorbidities and even death. As the majority of hypoglycemic cases are asymptomatic [25], enough emphasis should be given this subgroup.
At this juncture, an explanation of the cost-to-charge ratios (CCRs) is warranted. The HCUP KID contains data on total charges for each hospital in the databases. This charge information represents the amount that hospitals billed for services but does not reflect how much hospital services actually cost [23]. Cost information was obtained from the hospital accounting reports collected by the CMS. Statistical imputation for missing values and internal validation studies were carried out to enhance the accuracy of the CCRs [24]. Most hospital-based studies use total charge as a proxy measurement for actual cost [25]. This may lead to drawing unwarranted conclusions about economic efficiency and hospital resource utilizations [25]. To maximize the accuracy of the cost estimation, our study used a more accurate cost by converting the total hospital charge to hospital cost estimates using CCRs.
We recognize that there are some limitations associated with this study. The ICD-9-CM classification system is imperfect for case identification, as it was created for reimbursement rather than research purposes. As a result, important clinical conditions pertinent for outcome research may have been missed. Because KID 2012 lacks individual identifiers for states, we were not able to conduct comparative analysis among various states. However, despite the potential limitations, the HCUP KID database is the largest validated and publicly available all-payer pediatric inpatient care database [17] that can be used to evaluate national cost estimates, resource utilization, and economic burden of hospitalization in the pediatric population.
Conclusion
In conclusion, this study demonstrated that neonates with hypoglycemia consumed 11% of resources associated with hospital births while accounting for only 1.5% of hospitalization. We also demonstrated that hospital length of stay, hospital bed size, teaching hospitals, number of procedures performed, chronic conditions, comorbidity, prematurity, and in-hospital mortality were independently associated with increased hospital cost. Our results also suggested that non-premature hypoglycemic babies should be provided with more care to reduce acute comorbidities and death during hospitalization.
References
- Rozance PJ, Hay WW. Describing hypoglycemia-definition or operational threshold?. Early Human Development. 2010;86:275-280.
- Najati N, Saboktakin L. Prevalence and underlying etiologies of neonatal hypoglycemia. Pakistan J Biol Sci 2010;13:753.
- Rozance PJ, Hay WW. Hypoglycemia in newborn infants: Features associated with adverse outcomes. Neonatology 2006;90:74-86.
- Ramos GA, Hanley AA, Aguayo J, et al. Neonatal chemical hypoglycemia in newborns from pregnancies complicated by type 2 and gestational diabetes mellitus the importance of neonatal ponderal index. J Matern Fetal Neonatal Med 2012;25:267-271.
- Cornblath M, Ichord R. Hypoglycemia in the neonate. Semin Perinatol 2000;24;136-149.
- Lubchenco LO, Bard H. Incidence of hypoglycemia in newborn infants classified by birth weight and gestational age. Pediatrics 1971;47:831-838.
- Stanley CA, Baker L. The causes of neonatal hypoglycemia. N Engl J Med 1999;340:1200-1201.
- Holtrop PC. The frequency of hypoglycemia in full-term large and small for gestational age newborns. Am J Perinatol 1993;10:150-154.
- Hawdon JM. Hypoglycaemia and the neonatal brain. Eur J Pediatr 1999;158:S9-12.
- Agrawal RK, Lui K, Gupta JM. Neonatal hypoglycemia in infants of diabetic mothers. J Paediatr Child Health 2000;36:354-356.
- Gallo F, Maggi D, Cordera R. The economic burden of severe hypoglycemia: Two sides of the same coin. Comment on G. Veronese and Coll. Costs associated with emergency care and hospitalization for severe hypoglycemia. Nutrition, Metabolism and Cardiovascular Diseases: NMCD. 2016.
- Moisan J, Breton MC, Villeneuve J, et al. Hypoglycemia related emergency department visits and hypoglycaemia related hospitalizations among new users of anti-diabetes treatments. Can J Diabetes. 2013;37:143-149.
- Liu S, Zhao Y, Hempe JM, et al. Economic burden of hypoglycemia in patients with type 2 diabetes. Expert Rev Pharmacoeconomics Outcomes Res 2012;12:47-51.
- Zhao Y, Shi Q, Wang Y, et al. Economic burden of hypoglycemia: Utilization of emergency department and outpatient services in the United States (2005-2009). J Med Econ 2016;pp:1-6.
- Zhang Y, Wieffer H, Modha R, et al. The burden of hypoglycemia in type 2 diabetes: A systematic review of patient and economic perspectives. JCOM 2010;17:547-557.
- Kim G, Lee YH, Han MH, et al. Economic burden of hypoglycemia in patients with type 2 diabetes mellitus from Korea. PloS one 2016;11:e0151282.
- Healthcare Cost and Utilization Project. HCUP kids’ inpatient database. Agency for Healthcare Research and Quality: Rockville, MD. 2012.
- Hosmer DW, Taber S, Lemeshow S. The importance of assessing the fit of logistic regression models: A case study. Am J Public Health 1991;81:1630-1635.
- Daniel WW. Biostatistics: A foundation for analysis in the health sciences. John Wiley and Sons. Inc, New York, NY. 1995.
- Zenk KE. Neonatology: Management, procedures, on-call problems, diseases and drugs. Gomella TL, Cunningham MD, Eyal FG, editors. New York: McGraw-Hill 2004.
- Straussman S, Levitsky LL. Neonatal hypoglycemia. Current Opinion in Endocrinology, Diabetes and Obesity 2010;17:20-24.
- Kline GA, Edwards A. Antepartum and intra-partum insulin management of type 1 and type 2 diabetic women: Impact on clinically significant neonatal hypoglycemia. Diabetes Res Clin Pract 2007;77:223-230.
- www.hcup-us.ahrq.gov/db/state/costtocharge.jsp.
- Song X, Friedman B. Calculate cost adjustment factors by APR-DRG and CCS using selected states with detailed charges. HCUP Methods Series Report 2008;p:4.
- Finkler SA. The distinction between cost and charges. Annals of Internal Medicine. 1982;96:102-109.