Current Pediatric Research
International Journal of Pediatrics
Diagnostic role of serum prolactin in pediatric convulsions: A cross-sectional study.
Ronak Trikmani, Devang Gandhi*, Umang Patel
Department of Pediatrics, SMIMER Medical College, Veer Narmad South Gujarat University, Gujarat, India
- *Corresponding Author:
- Devang Gandhi
Department of Pediatrics,
SMIMER Medical College, Veer Narmad South Gujarat University,
Gujarat,
India
E-mail: drdevang1981@gmail.com
Received: 27 February, 2024, Manuscript No. AAJCP-25-163082; Editor assigned: 01 March, 2024, Pre QC No. AAJCP-25-163082 (PQ); Reviewed: 15 March, 2024, QC No. AAJCP-25-163082; Revised: 06 March, 2025, Manuscript No. AAJCP-25-163082 (R); Published: 03 April, 2025, DOI:10.35841/0971-9032.29.01.2359-2362.
Introduction: Seizures in children are a major neurological concern, with causes ranging from febrile convulsions to epilepsy and metabolic imbalances. Serum prolactin, a hormone linked to stress responses, has been explored as a potential biomarker for differentiating epileptic from non-epileptic seizures. This study aims to assess the diagnostic reliability of serum prolactin levels in various pediatric convulsions. Materials and methods: This cross-sectional study was conducted at a teaching hospital in South Gujarat, India, including 121 children aged 6 months to 18 years with convulsions. Serum prolactin levels were measured within 6 hours of seizure onset before anticonvulsant therapy. Data were analyzed using statistical software SPSS version 21.2. Results: In our study, serum prolactin levels were significantly associated with convulsion types (p<0.001), highest in status epilepticus (66.7%) and GTCS (63.8%). Measurement timing also influenced levels in GTCS (p=0.011); 69.2% were elevated within 3 hours, dropping to 16.7% after. Outcomes were linked to convulsion type (p=0.04); febrile (97.5%) and focal aware convulsions (90.9%) had the highest discharge rates, while GTCS (25.9%) and status epilepticus (33.3%) had the highest DAMA rates. Mortality was highest in focal impaired-awareness convulsions (22.2%) and GTCS (6.9%). Serum prolactin levels were also associated with discharge outcomes (p=0.03), with increased levels in 27.9% of DAMA cases and 4.7% of deaths. Conclusion: Serum prolactin is a key marker in pediatric convulsions, particularly in GTCS and status epilepticus, indicating greater seizure severity.
Abstract
Introduction: Seizures in children are a major neurological concern, with causes ranging from febrile convulsions to epilepsy and metabolic imbalances. Serum prolactin, a hormone linked to stress responses, has been explored as a potential biomarker for differentiating epileptic from non-epileptic seizures. This study aims to assess the diagnostic reliability of serum prolactin levels in various pediatric convulsions.
Materials and methods: This cross-sectional study was conducted at a teaching hospital in South Gujarat, India, including 121 children aged 6 months to 18 years with convulsions. Serum prolactin levels were measured within 6 hours of seizure onset before anticonvulsant therapy. Data were analyzed using statistical software SPSS version 21.2.
Results: In our study, serum prolactin levels were significantly associated with convulsion types (p<0.001), highest in status epilepticus (66.7%) and GTCS (63.8%). Measurement timing also influenced levels in GTCS (p=0.011); 69.2% were elevated within 3 hours, dropping to 16.7% after. Outcomes were linked to convulsion type (p=0.04); febrile (97.5%) and focal aware convulsions (90.9%) had the highest discharge rates, while GTCS (25.9%) and status epilepticus (33.3%) had the highest DAMA rates. Mortality was highest in focal impaired-awareness convulsions (22.2%) and GTCS (6.9%). Serum prolactin levels were also associated with discharge outcomes (p=0.03), with increased levels in 27.9% of DAMA cases and 4.7% of deaths.
Conclusion: Serum prolactin is a key marker in pediatric convulsions, particularly in GTCS and status epilepticus, indicating greater seizure severity.
Keywords
Serum prolactin, Pediatric convulsions, GTCS, EEG abnormalities, Seizure prognosis.
Introduction
Seizures in children are a significant neurological concern, with multiple underlying causes ranging from febrile convulsions to epilepsy and metabolic imbalances [1]. Identifying biomarkers that can aid in the differentiation between epileptic and non-epileptic seizures remains an essential focus in pediatric neurology [2].
Elevated prolactin levels following a convulsive episode may serve as a useful biochemical marker for distinguishing true epileptic seizures from Psychogenic Non-Epileptic Seizures (PNES) or other mimicking conditions [3].
Several studies have explored the variations in serum prolactin levels post-seizure, indicating that significant elevation occurs within 10-20 minutes of an epileptic event [4]. This transient rise is believed to be mediated by neuronal activation in the hypothalamic-pituitary axis during generalized or focal seizures with impaired awareness [5].
Materials and Methods
Study setting
This study was conducted in a teaching hospital located in South Gujarat, India, specifically within the Paediatric Intensive Care Unit (PICU) and the general paediatric ward.
Study population
The study population included all children aged 6 months to 18 years who presented with active convulsions or had a history of convulsions and met the inclusion criteria. These children were admitted to the hospital during the study period.
Study design
The study utilized a cross-sectional design, aiming to investigate the association between S. PRL levels and different types of convulsions in children.
Study duration
The study was conducted over a period of 18 months, during which data were collected from eligible patients.
Sample size
The sample size for this study was determined to be 121 children. The sample size was calculated using the following assumptions and formula:
The sample size was calculated considering the proportion of seizures (13.1%; 30/229) among the total admitted patients in PICU at tertiary care hospitals from the last six months of data recorded.
P=13.1%
q=1-p
Zα/?=Level of confidence=95%
L=Allowable error=6%

Inclusion criteria
• Children aged 6 months to 18 years with convulsions or a history of convulsions and admitted to the hospital.
• Children admitted for any disease who developed convulsions during their hospital stay.
• Patients whose S. PRL levels were measured in external hospitals for prior episodes of convulsions but not in the current hospital.
Exclusion criteria
• Patients whose S. PRL levels were already measured in the hospital during prior episodes of convulsions.
• Patients on medications known to alter PRL levels (e.g., typical and atypical antipsychotics, tricyclic antidepressants, insulin, MAO inhibitors phenytoin, metoclopramide, domperidone).
• Patients who had more than two episodes of convulsions within 24 hours before admission. This criterion is based on evidence indicating that the postictal rise in PRL is diminished when seizures occur after short seizure-free intervals of <24 hours.
Serum prolactin analysis followed sex-specific cut-offs: 11 ng/mL (234 mIU/L) for males and 20 ng/mL (425.532 mIU/L) for females. Statistical analyses using IBM SPSS version 21.2 included descriptive and inferential tests (chi-square), with a significance threshold of p<0.05.
Results
In our study, 64% of participants were males and 36% females. Age showed a significant association with serum prolactin levels (p<0.001); 70% of children with increased levels were aged 5-12 years. Among those with normal levels, 47% were 5-12 years and 46% were 6 months 5 years. Age also correlated with convulsion type (p<0.001); GTCS was most common in the 12-18 year (84.6%) and 5-12 year (64.2%) groups, while febrile convulsions prevailed in 6 months 5 years (82.9%). Sex distribution was significant (p<0.01); males had 27% increased and 73% normal levels, while females had equal proportions.
Serum prolactin levels were significantly associated with convulsion types (p<0.001), with increases in status epilepticus (66.7%) and GTCS (63.8%), while 95% of febrile convulsions had normal levels. Measurement timing also influenced levels in GTCS (p=0.011); 69.2% had increased levels within 3 hours, dropping to 16.7% after 3 hours. Febrile and focal aware convulsions mostly had normal levels, regardless of timing (p=0.504, p=0.621). Status epilepticus consistently showed increased levels within 3 hours, while focal impairedawareness convulsions had no increased cases (Table 1).
| Convulsion type | Serum prolactin levels (increased) | Serum prolactin levels (normal) | Total (N%) |
|---|---|---|---|
| Febrile convulsion | 2 (5.00%) | 38 (95.00%) | 40 (100.00%) |
| Focal aware convulsion | 2 (18.20%) | 9 (81.80%) | 11 (100.00%) |
| Focal convulsion with impaired awareness | 0 | 9 (100.00%) | 9 (100.00%) |
| GTCS | 37 (63.80%) | 21 (36.20%) | 58 (100.00%) |
| Status epilepticus | 2 (66.70%) | 1 (33.30%) | 3 (100.00%) |
| Total | 43 (35.50%) | 78 (64.50%) | 121 (100.00%) |
Table 1. Serum prolactin levels by convulsion types.
In our study, 43% (N=52) of children underwent MRI, with 44% (N=23) showing abnormalities. No significant association was found between serum prolactin levels and MRI results. Elevated prolactin was seen in 61% of abnormal and 52% of normal MRI cases. Prolactin levels were significantly associated with MRI findings based on convulsion types (p=0.015, p=0.008). Among normal MRI cases, increased prolactin was found in 72% of GTCS and 40% of focal aware convulsions, while none of the focal impaired-awareness cases showed elevation (Table 2).
| Convulsion type by abnormal MRI | Serum prolactin increased | Serum prolactin normal | Total (N%) | P-Value |
|---|---|---|---|---|
| Focal aware convulsion | 4 (100.0%) | 0 (0.0%) | 4 (100.0%) | 0.015 |
| Focal convulsion with impaired awareness | 1 (100.0%) | 0 (0.0%) | 1 (100.0%) | |
| GTCS | 12 (75.0%) | 4 (25.0%) | 16 (100.0%) | |
| Status epilepticus | 2 (100.0%) | 0 (0.0%) | 2 (100.0%) | |
| Total | 14 (60.9%) | 9 (39.1%) | 23 (100.0%) |
Table 2. Serum prolactin levels by convulsion type for abnormal MRI findings.
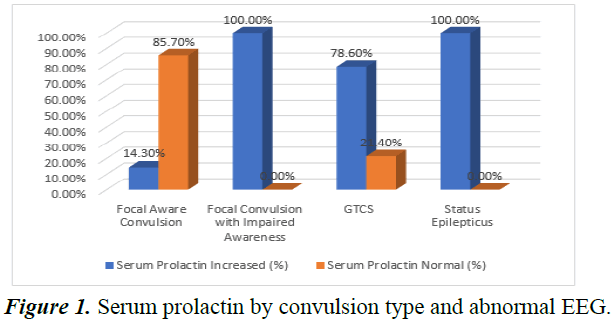
In our study, 57% (N=69) of children underwent EEG, with 64% (N=44) showing abnormalities. Serum prolactin was elevated in 56.8% of abnormal EEG cases and 36.0% of normal EEG cases, but the association was not statistically significant (p=0.09) (Figure 1).
Serum prolactin levels were not significantly associated with convulsion types in normal EEG cases (p=0.23). Elevated levels appeared in 53.3% of GTCS and all cases of focal impaired-awareness convulsions and status epilepticus, while febrile and focal aware convulsions mostly had normal levels. Outcomes were significantly linked to convulsion types (p=0.04); most febrile (97.5%) and focal aware (90.9%) cases were discharged. DAMA rates were highest in GTCS (25.9%) and status epilepticus (33.3%), while mortality was most frequent in focal impaired-awareness convulsions (22.2%) and GTCS (6.9%) (Table 3).
| Outcome | Serum prolactin increased (%) | Serum prolactin normal (%) | Total (%) | P-value |
|---|---|---|---|---|
| DAMA | 27.90% | 10.30% | 16.50% | 0.03 |
| Death | 4.70% | 2.60% | 3.30% | |
| Discharge | 67.40% | 87.20% | 80.20% |
Table 3. Serum prolactin levels by discharge outcome.
Discussion
Serum prolactin levels were significantly associated with convulsion types, highest in status epilepticus and GTCS, while 95% of febrile convulsions had normal levels. This aligns with Kumari et al., who reported higher post-ictal levels in GTCS and and Mishra et al., who found elevated levels in epileptic seizures but normal levels in febrile seizures and mimics [6,7].
Prolactin measurement timing also influenced levels, particularly in GTCS; 69.2% had elevated levels within 3 hours, dropping to 16.7% after Wani et al. found prolactin peaked within 20 minutes, while Rehana et al., and Chaudhary et al. reported sustained elevation in GTCS and CPS compared to febrile convulsions, supporting our findings that GTCS and status epilepticus had consistently high levels within 3 hours [7-9].
In our study, 43% of children underwent MRI, with 44% showing abnormalities, but no significant association with serum prolactin levels was found. This aligns with Kumari et al. and Mishra et al., who reported elevated prolactin in GTCS and focal seizures but no strong correlation with MRI findings. Wang et al., noted that prolactin reflects postictal hypothalamic activation rather than structural changes, while Rehana et al., found MRI abnormalities more common in epilepsy but unrelated to prolactin levels [10].
For EEG, 57% of children were tested, with 64% showing abnormalities. Elevated prolactin was found in 56.8% of abnormal EEG cases and 36.0% of normal cases, though not statistically significant. Kumari et al., reported similar inconsistencies in EEG correlation. Rehana et al., highlighted EEG as the gold standard for epilepsy, with prolactin serving as a supportive but limited marker. Wang et al., noted prolactin levels depend on seizure type and duration rather than EEG abnormalities, explaining the weaker association.
Patient outcomes showed a significant association with convulsion types. Febrile and focal aware convulsions had the highest discharge rates, while GTCS and status epilepticus had the highest DAMA rates. Mortality was most common in focal impaired-awareness convulsions and GTCS. Kumari et al., reported similar trends, with febrile convulsions having the best prognosis, while GTCS and status epilepticus had higher complications and DAMA cases. Mishra et al., linked mortality to focal seizures with impaired awareness due to neurological comorbidities. Rehana et al., noted higher DAMA rates in GTCS due to prolonged hospital stays, while Wang et al., confirmed worse outcomes in status epilepticus, supporting our findings.
Limitations include a small sample size affecting generalizability, varied timing of serum prolactin measurement and unaccounted factors like stress, medications and endocrine disorders. While EEG and MRI findings were analyzed, their correlation with outcomes requires further study.
Conclusion
Serum prolactin levels play a significant role in assessing pediatric convulsions, particularly in GTCS and status epilepticus, where elevated levels indicate greater seizure severity. While not strongly associated with MRI findings or lapse time, prolactin correlated with abnormal EEG results and poorer outcomes, including higher mortality rates.
References
- van Baalen A, Vezzani A, Hausler M, et al. Febrile infection-related epilepsy syndrome: Clinical review and hypotheses of epileptogenesis. Neuropediatrics 2017; 48: 5-18.
[Crossref] [Google Scholar] [PubMed]
- Whelan H, Harmelink M, Chou E, et al. Complex febrile seizures: A systematic review. Dis Mon 2017; 63: 5-23.
- Bajestan SN, LaFrance Jr WC. Clinical approaches to psychogenic nonepileptic seizures. Focus 2016; 14: 422-431.
[Crossref] [Google Scholar] [PubMed]
- Rider F, Turchinets A, Druzhkova T, et al. Dissimilar changes in serum cortisol after epileptic and psychogenic non-epileptic seizures: A promising biomarker in the differential diagnosis of paroxysmal events? Int J Mol Sci 2024; 25: 7387.
[Crossref] [Google Scholar] [PubMed]
- Wulsin AC, Solomon MB, Privitera MD, et al. Hypothalamic-pituitary-adrenocortical axis dysfunction in epilepsy. Physiol Beh 2016; 166: 22-31.
[Crossref] [Google Scholar] [PubMed]
- Kumari P, Paul S, Sk MR, et al. Diagnostic role of serum prolactin level in different kinds of seizure and seizure-like episode in children: A hospital-based study. Asian J Med Sci 2024; 15: 191–195.
- Mishra R, Chaudhary BN. Study of the levels of serum prolactin in childhood seizure disorder. IOSR J Dent Med Sci 2017; 16: 48-50.
- Wani AA, Shabir S, Bhat IA. Study of serum prolactin levels in seizures list of authors in order. Int J Med Sci Curr Res 2019; 2: 275-287.
- Rehana KA, Irshad M, Ashraf M. Role of serum prolactin levels in diagnosis of epileptic and pseudoepileptic events in children, a tertiary care experience. Int J Contemp Med Res 2019; 6.
- Wang YQ, Wen Y, Wang MM, et al. Prolactin levels as a criterion to differentiate between psychogenic non-epileptic seizures and epileptic seizures: A systematic review. Epilepsy Res 2021; 169: 106508.
[Crossref] [Google Scholar] [PubMed]