Current Pediatric Research
International Journal of Pediatrics
Diagnose of plantar psoriasiform leishmaniasis with use of dermoscope: A case report.
Elloudi S*, Ammari S, Bay Bay H, Douhi Z, Mernissi FZ
Department of Dermatology and Venereology, Sidi Mohamed Ben Abdellah University, Fès, Morocco
- *Corresponding Author:
- Elloudi S
Department of Dermatology and Venereology
Sidi Mohamed Ben Abdellah University
Fès
Morocco
E-mail: dr.elloudi@gmail.com
Received: 25 November, 2022, Manuscript No. AAJCP-22-47687; Editor assigned: 28 November, 2022, Pre QC No. AAJCP-22-47687(PQ); Reviewed: 12 December, 2022, QC No. AAJCP-22-47687; Revised: 22 December, 2022, Manuscript No. AAJCP-22-47687(R); Published: 30 December, 2022, DOI:10.35841/0971-9032.27.01.1759-1761.
Cutaneous leishmanias is a great simulator either by its clinical aspect, or by its location. We report the observation of a child who presented with psoriasiform and plantar impetiginoid plaque progressing for 3 months, first suggesting plantar psoriasis. The dermoscopic examination reoriented the diagnosis by objectifying salmon areas related to a granulomatous infiltrate. The smear confirmed the presence of leishmanian bodies. The plaque completely regressed after treatment with intralesional pentavalent antimony. The psoriasiform appearance, as well as the plantar location was puzzling elements, however, the dermoscope was a very useful tool in guiding the diagnosis.
Keywords
Plantar leishmaniasis, Atypical forms, Dermoscopy
Introduction
Localized cutaneous leishmaniasis is a parasitic infection caused by a protozoan of the genus leishmania, usually localized in an uncovered area corresponding to the site of inoculation by the bite of the sand-fly. Cutaneous leishmaniasis is generally easy to recognize, however, there are some unusual forms which pose a diagnostic challenge. These deceptive forms can be related to the clinical appearance, or even related to the topography of the lesion. Plantar localization is very rare; we report a case with a clinical psoriasiform appearance.
Case Presentation
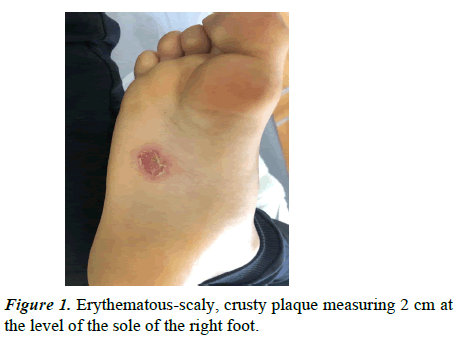
This is a 9-year-old child, with no notable pathological history, who presented with an asymptomatic plantar lesion, progressing 3 months before his consultation. Dermatological examination found a crusty, erythematous scaly plaque measuring 2 cm on the sole of the right foot (Figure 1).
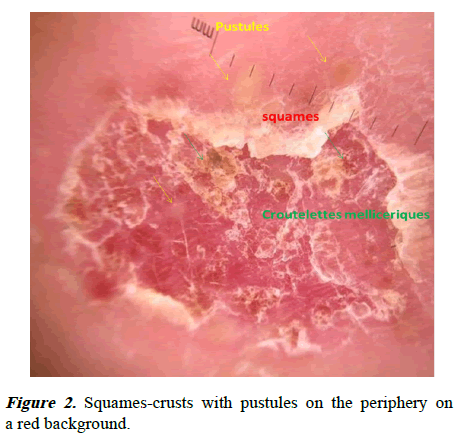
Dermoscopy revealed a very inflammatory background, punctiform erosions, and scaly scales with pustules on the periphery (Figure 2)
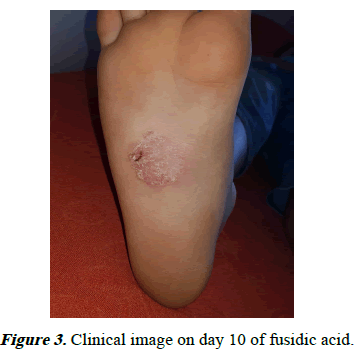
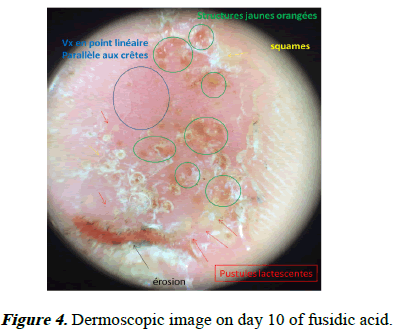
It was thought first of an impetiginized plantar psoriasis, and it was preferred to treat locally with Fusidic acid and control the patient after 10 days. Indeed at dermoscopic control, we objectified whitish scales, pustules, vessels in point parallel to the ridges (Figures 3 and 4) still suggesting the diagnosis of psoriasis, but we were able to detect yellow-orange-salmon structures very suggestive of a granulomatous infiltrate. A skin smear was carried out objectifying the presence of leishmania bodies. The diagnosis was therefore localized cutaneous plantar psoriasiform leishmaniasis.
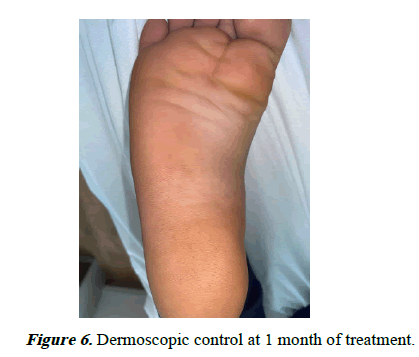
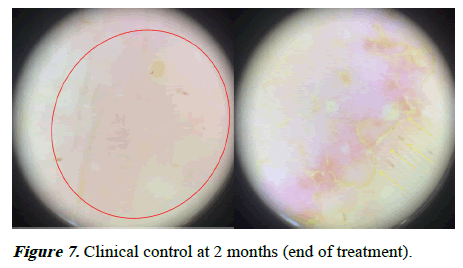
We opted for intra-lesional treatment with pentavalent antimony 2 ml three times a week for 2 months combined with aureomycin ointment 3%. Clinical and dermoscopic control at 1 month after the start of treatment showed the persistence of a progressive border (Figures 5 and 6), hence the need to extend treatment to 2 months (Figure 7). The plaque completely regressed without recurrence with a follow-up of 2 years.
Results and Discussion
Cutaneous leishmaniasis is a great simulator by its clinical aspects or sometimes by some misleading localizations. The plantar location is exceptional because it is an undiscovered area on the one hand, and on the other hand, the thickness of the stratum corneum in this area makes inoculation of the parasite by the vector difficult [1]. In a series of 10,850 cases reported by the Tunisian team, palmarplantar localization was reported only in 0.41% of cases, with 24 palmar cases, 9 plantar cases and 2 cases of palmoplantar localization [2]. Several atypical clinical aspects have been described in the previous literature including the psoriasiform and impetigenoid form, as was the case in our patient [2-4].
In the face of these unusual clinical aspects, dermoscopy is a very useful tool in guiding the diagnosis [5]. Several dermoscopic patterns have been described in the previous literature, however, the demonstration of salmon structures is a key element in the diagnosis [6,7].
In our patient, although the initial clinical and dermoscopic appearance of the lesion suggested the diagnosis of localized and impetiginized psoriasis, evaluation and dermoscopic control was necessary, thus orienting the diagnosis towards a granulomatous pathology, in particular leishmaniasis. The diagnosis is confirmed by the revelation of the leishmania bodies in the skin smear, if necessary, by their demonstration by a special staining in histology with the presence of tuberculoid granulomas without caseous necrosis [1,8].
Conclusion
In conclusion, cutaneous leishmaniasis is a large simulatrice characterized by clinical polymorphism, even trompeur. The location plantaire is three rare and is recognized by clinicians. In our case, we opted for an intra-lesional treatment with a good evolution and a follow-up of 2 years without recurrence. In patient perspective the patient claimed his satisfaction with the good evolution of his condition after treatment. Pentavalent antimony is the first-line treatment that can be administered intravenously, intramuscularly or intralesion depending on the number, location and diameter of the lesions.
Ethical Approval
The patient was informed and gave their informed consent.
Acknowledgements
We are indebted to the patient, who gave us his consent for publication.
Conflict of Interests
The authors declared no potential conflicts of interest.
Funding
The authors declare that they have no funding.
Consent for Publication
Written informed consent was obtained from the patient for publication of his case report and any accompanying images. A copy of the written consent is available for review by the editorin- chief of this journal.