Current Pediatric Research
International Journal of Pediatrics
Colon atresia: Rare cause of neonatal bowel obstruction.
D. Hanine*, M. Hadir, A. Skiredj, L. El Aqqaoui, H. Oubejja, H. Zerhouni, F. Ettayebi
Department of Pediatric Surgery Emergencies, Mohammed V University, Rabat, Morocco
- Corresponding Author:
- D. Hanine
Department of Pediatric Surgery Emergencies,
Mohammed V University,
Rabat,
Morocco,
E-mail: h.driss207@hotmail.com
Received: 19 May, 2024, Manuscript No. AAJCP-24-12831; Editor assigned: 22 May, 2024, Pre QC No. AAJCP-24-12831 (PQ); Reviewed: 05 June, 2024, QC No. AAJCP-24-12831; Revised: 01 September, 2024, Manuscript No. AAJCP-24-12831 (R); Published: 29 September, 2024, DOI: 10.35841/0971-9032.28.09.2342-2345.
Colonic atresia is the least common atresia of the digestive system. Antenatal vascularization disorder is the most common etiological hypothesis commonly accepted to explain complete forms. This anomaly can be isolated or part of a poly malformation syndrome. We report a rare case of colon atresia admitted to a low neonatal occlusion table, negative probe test. The surgical exploration objectified a type I colic atresia. The patient underwent a first colostomy then an end-to-end anastomosis, with good operating suites. In the light of this observation and after a review of the literature; we emphasize the rarity of the pathology and the difficulty of treatment, especially in the event of delayed diagnosis.
Keywords
Colon, Atresia, Neonatal obstruction
Introduction
Colonic atresia is a rare birth defect. It is defined by the congenital absence of light in the colon. It only represents 1.8% to 15% of all intestinal atresia. Its association with hail atresia is exceptional. It is a neonatal emergency that produces a low occlusion table with a risk of intestinal perforation involving life-threatening.
The diagnostic approach is essentially based on radiological examinations. Surgical treatment remains controversial as evidenced by the great diversity of indications found in the literature. The prognosis depends not only on the earliness and quality of treatment but also on the severity of the malformations associated with CA. This work consists of a review of the literature on colic atresia, with a brief presentation and some reflections concerning the management of this condition [1-3].
Case Presentation
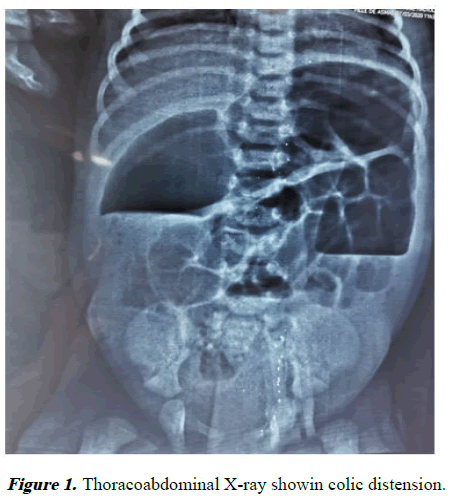
Our study was done in January 2020 at the pediatric surgery emergencies department at the Children's Hospital of Rabat, the case studied is a female newborn, who has 4-day-old brought by her parents with an acute bowel obstruction. The history of the disease takes back to birth by non-emission of meconium with bilious vomiting and abdominal distension. The probe test was negative. Biological assessments returned normal. The thoraco-abdominal x-ray showed an obvious dilation of the transverse and descending colon (Figure 1) [4-6].
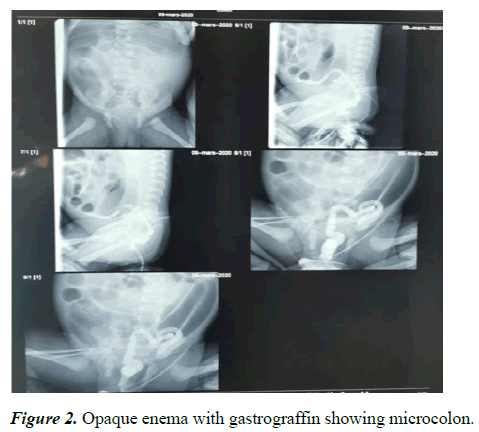
A Hirschprung disease spread beyond the sigmoid region has been evocated. A gastrograffin index x-ray for diagnostic purposes was carried out, objectifying a non-functioning microcolon (Figure 2) [7].
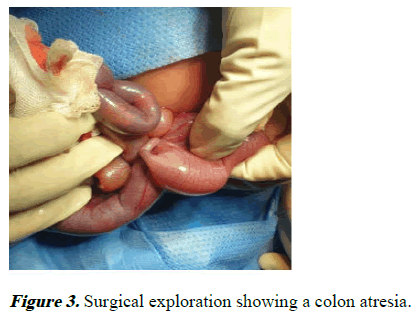
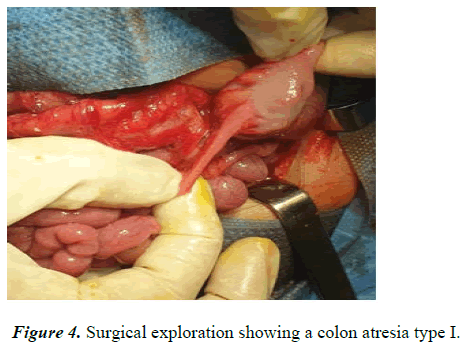
Until now, surgical exploration is required. During surgical exploration, there is a disparity in caliber in the descending colon with type I colic atresia. (Figures 3 and 4). A colostomy was performed in order to relieve the newborn, then a resumption of surgery with resection of the atretic part and endto- end anastomosis. The operating suites were simple with good progress [8].
Results and Discussion
CA is defined by the congenital absence of light in the colon. There are three types according to Louw's classification. Another classification has been proposed by Grosfeld and his collaborators. Whatever the type of atresia, the pathological changes due to the obstruction are the same. Several theories have been put forward trying to explain the etiopathogenesis of colonic atresia: Vascular, genetic, infectious and malformative theory [9].
Colonic atresia is one of the rare causes of neonatal obstructions. They represent 1.8% to 15% of all digestive atresias. Their incidence has been estimated at 1 in 1,500 to 20,000 live births. They are most often observed in term newborns and both sexes are equally affected. These atresias are isolated in 2/3 of the cases, but can be associated with various malformations. We quote: Hirschprung's disease or Congenital Megacolon (MCC): It is rarely associated with CA. This association is found in 2% of newborns, it is more frequent in case of type III atresia. The diagnosis of MCC is often made following the failure to restore colonic continuity after radical treatment of CA (release of the anastomosis, occlusion). Conventionally, the association of Hirschprung's disease is suspected before malrotation or a defect in the fixation of the colon underlying atresia and must be confirmed by performing rectal biopsies objectifying the absence of cells lymph nodes in the submucosal plexus associated with Schwannian hyperplasia. According to recent data, the association of a MCC must be systematically sought whatever the orientation or the fixation of the distal colon before the closure of the colostomy, thus avoiding any postoperative complication and a possible resumption of surgery. other intestinal malformations: Jejunal, ileal atresia, colic, neuronal intestinal dysplasia, anal imperforation, congenital segmental dilation of the colon. Anomalies in the fixation of the mesentery. Anomalies of the abdominal wall: omphalocele, laparoschisis. More rarely: Ocular malformations (exophthalmos, anophthalmos, optic nerve hypoplasia), craniocerebral, facial cardiac, urinary, musculoskeletal and varicella fetal syndrome, vascular. Regarding the prenatal diagnosis, it is difficult to make since generally there are no hydramnios; obstetric ultrasound can visualize colonic distension without being able to relate it to atresia, it can also objectify an isolated ascites. In the neonatal period, colonic atresia clinically produces a low neonatal occlusion table. The first signs may not appear until after 24 hours of life and sometimes even later. As in the case of our patient. Radiological examinations remain the essential time of the diagnostic process abdomen without preparation has only orientation value. The diagnosis of certainty is made by the opaque enema [10].
It specifies the seat and the type of atresia:
• The pathognomonic image of CA results in a distal
microcolon with complete stop of the opaque column and
without passage towards the dilated upstream segments.
• Certain radiological signs make it possible to recognize the
type of atresia in question according to Louw's
classification.
A distinction is thus made:
• The wind-sock sign
• The hook sign
The differential diagnosis is that of other causes of low neonatal obstruction. During surgical exploration, the dilated handles are exteriorized in order to access the atretic area. The local state must be carefully assessed in search of areas of intestinal suffering (cyanosis, necrosis) or possible perforation. The entire small intestine and colon must be explored in order to find any associated abnormality. The MCC must be systematically sought regardless of the orientation or fixation of the distal colon by performing an extemporaneous. Finally, the choice between an anastomosis resection or a simple first derivation varies according to the authors:
• The principle of radical surgery is to remove the obstacle
and restore intestinal continuity. The resection must relate
to the atretic zone and the proximal and distal colic ends
whose vascularization and the innervation are pathological.
• In the event of a first diversion, the restoration of colonic
continuity takes place within a few months of the
colostomy.
Surgical treatment of AC is not perfectly codified as evidenced by the great diversity of indications found in the literature. This is due to the rarity of this malformation preventing the use of controlled prospective studies to assess the value of a particular treatment. Classically, the choice between a treatment in one or in two stages, depends on the majority of the authors of two main parameters: The general condition of the newborn. The topography of atresia.
Thus, a first diversion makes it possible to quickly remove the obstacle and postpone the cure for atresia to a better time (2 to 3 months later) in the following situations:
• A deterioration in the general state: Materno-fetal infection,
delayed diagnosis, associated malformations.
• A right CA with the presence of signs of ischemia or
perforation requiring a right colectomy with ileostomy or
when the ascending colon is very distended and an
anastomosis resection is difficult to perform given the great
disparity of sizes of the two proximal ends and distal.
• In angular-splenic aresesia, where the disparity in caliber
still considerable between the colonic extremities makes an
anastomosis difficult from the start. Very often the dilation
is uniform over the entire colon upstream of atresia, so that
resection of the entire colon upstream would make an
excessive colonic sacrifice.
• The most logical attitude is to perform a double colostomy.
This allows, on the one hand, to remove the obstacle and
authorize oral feeding; and on the other hand to irrigate the
distal colon in order to increase its caliber and facilitate
subsequent anastomosis. The exteriorization of the two
colonic extremities by the same parietal orifice, whenever
possible, allows a few weeks later, the restoration of
continuity by elective means.
Metabolic monitoring of these colostomies is less cumbersome than that of small bowel movements. The treatment in only one time is carried out in the preangulosplenic atresia, in a new born in good general condition. Termino-terminal ileocolic anastomosis is easily performed because the caliber disparity between the ileal and colonic extremity is small and modeling is rarely necessary [11,12].
In more recent series and whenever the general condition of the newborn allows, treatment in one time was performed without taking into account the headquarters of the CA. Indeed, several authors prefer a primary anastomosis if the disparity in size between the proximal and distal ends is minimal (ratio proximal/distal diameter 3/1) and if no other cause of mechanical or functional distal obstruction is associated with the colic atresia. In these cases, the AC cure is performed without prior bypass. This is a new concept in colon atresia surgery which is developing and which claims to reduce the risks associated with anesthesia and iterative surgical procedures [13,14]. This concept has benefited from considerable progress in neonatal resuscitation.
Conclusion
Colic atresia remains a rare congenital malformation, but which must be known by the pediatric surgeon in view of the risk of life-threatening intestinal perforation. It’s a rare neonatal emergency. Interest of digestive clouding in front of any low neonatal occlusion. Its surgical treatment is not perfectly codified and can be carried out in one or two stages depending on several parameters. A radical treatment offered right away seems to be potentially beneficial. Its prognosis remains excellent in the event of early management and in the absence of associated severe malformations.
Conflict of Interest
All authors have contributed to the writing of this manuscript and all declare that they have no conflict of interest.
References
- Etensel B, Temir G, Karkiner A, et al. Atresia of the colon. J Pediatr Surg 2005; 40: 1258-1268.
[Crossref] [Google Scholar] [PubMed]
- Karnak I, Ciftci AO, Senocak ME, et al. Colonic atresia: Surgical management and outcome. Pediatr Surg Int 2001; 17: 631-635.
[Crossref] [Google Scholar] [PubMed]
- Komuro H, Urita Y, Hori T, et al. Perforation of the colon in neonates. J Pediatr Surg 2005; 40: 1916-1919.
[Crossref] [Google Scholar] [PubMed]
- Cox SG, Numanoglu A, Millar AJ, et al. Colonic atresia: Spectrum of presentation and pitfalls in management. A review of 14 cases. Pediatr Surg Int 2005; 21: 813-818.
[Crossref] [Google Scholar] [PubMed]
- Helardot P, Bienayme J, Bargy F, et al. Digestive surgery for children. Doin 1990.
- Watts AC, Sabharwal AJ, MacKinlay GA, et al. Congenital colonic atresia: Should primary anastomosis always be the goal? Pediatr Surg Int 2003; 19: 14-17.
[Crossref] [Google Scholar] [PubMed]
- Grosfeld JL, Ballantine TV, Shoemaker R. Operative management of intestinal atresia and stenosis based on pathologic findings. J Pediatr Surg. 1979; 14(3): 368-375.
[Crossref] [Google Scholar] [PubMed]
- Dalla Vecchia LK, Grosfeld JL, West KW, et al. Intestinal atresia and stenosis: A 25-year experience with 277 cases. Arch Surg 1998; 133: 490-497.
[Crossref] [Google Scholar] [PubMed]
- Azzie G, Craw S, Beasley SW. Colonic atresia: From suspicion to confirmation on pre‐operative radiology. J Paediatr Child Health 2002; 38: 518-520.
[Crossref] [Google Scholar] [PubMed]
- Draus Jr JM, Maxfield CM, Bond SJ. Hirschsprung's disease in an infant with colonic atresia and normal fixation of the distal colon. J Pediatr Surg 2007; 42: 5-8.
[Crossref] [Google Scholar] [PubMed]
- Lauwers P, Moens E, Wustenberghs K, et al. Association of colonic atresia and Hirschsprung’s disease in the newborn: Report of a new case and review of the literature. Pediatr Surg Int 2006; 22: 277-281.
[Crossref] [Google Scholar] [PubMed]
- Seo T, Ando H, Watanabe Y, et al. Colonic atresia and Hirschsprung's disease: Importance of histologic examination of the distal bowel. J Pediatr Surg 2002; 37: 1-3.
[Crossref] [Google Scholar] [PubMed]
- Kim CW, Superina RA, Ein S. Colonic atresia combined with Hirschsprung's disease: A diagnostic and therapeutic challenge. J Pediatr Surg 1995; 30: 1216-1217.
[Crossref] [Google Scholar] [PubMed]
- Williams MD, Burrington JD. Hirschsprung's disease complicating colon atresia. J Pediatr Surg 1993; 28: 637-639.
[Crossref] [Google Scholar] [PubMed]