Current Pediatric Research
International Journal of Pediatrics
Clinical and lung ultrasonographic features of transient tachypnea of newborn in a tertiary care hospital in Bangalore
Shruthi Patel* and Chandrakala P
Department of Paediatrics, KIMS Bangalore, Karnataka, India
- *Corresponding Author:
- Shruthi Patel
Kempegowda Institute of Medical Sciences
No.211, 9th Main 1st block, HRBR Layout Kalyan Nagar
Bengaluru- 560043, Karnataka, India
Tel: 9743513163
E-mail: shruthi13p@gmail.com
Accepted on 10th June 2019
Introduction: Transient tachypnea of the newborn (TTN) also called wet lung, occurs due to delayed clearance of lung fluid. The diagnosis of TTN was primarily based on medical history, clinical manifestations, arterial blood gas analysis, and chest radiography (CXR). It is estimated that over 70% of infants with TTN are clinically misdiagnosed with Respiratory distress syndrome (RDS). Lung ultrasound (LUS) is an emerging technique that could be used for early detection of TTN. This study aims to evaluate the value of lung ultrasound in the diagnosis of TTN in late-preterm and full-term neonates.
Material and Methods: Sixty five late preterm and term neonates with signs of respiratory distress were included in this prospective observational study from January 2016 to June 2017. Lung ultrasound was done within the first 24 hours of birth and assessed according to the observation indices like A-line, B-line and Double lung point.
Results: On lung ultrasound, 53 (81.5%) neonates showed the feature of double lung point (DLP) while 41 (63.1%) neonates showed A-line. The respiratory symptoms subsided in 38 (58.4%) babies at room air while only 2 (3.1%) babies required continuous positive airway pressure ventilation. The DLP feature on LUS was significantly more in babies born to primi mothers than multigravida (p value 0.02) and those delivered through LSCS when compared to babies delivered vaginally (p value- 0.01).
Conclusion: TTN is a self-limiting condition and treatment is mainly supportive. The results of this study further demonstrate that LUS can accurately and reliably diagnose TTN. Therefore, significantly reducing the need for chest X-rays and ultimately result in lower exposure of a neonate to ionizing radiation. This will aid in counselling the parents regarding its benign nature and conservative management.
Keywords
Transient tachypnea of newborn, Lung ultrasonography, Double lung point.
Introduction
Lung diseases are the most common conditions in newborn infants and children and are also the primary causes of death in children younger than 5 years [1,2]. A wide variety of pathologic lesions may cause respiratory disturbance in newborn including respiratory distress syndrome (RDS), transient tachypnea of newborn(TTN), pneumonia, sepsis, pulmonary hypertension, meconium aspiration, cyanotic congenital heart disease, congenital malformations (e.g., congenital diaphragmatic hernia, cystic adenomatoid malformations), central nervous system (CNS) insults (subarachnoid hemorrhage, hypoxic-ischemic encephalopathy) causing central hyperventilation, pneumothorax, polycythemia, and metabolic acidosis [3]. Hence, accurate and timely diagnosis is extremely important in order to enable efficient treatment and improve the prognosis of patient with lung disease. Lately lung ultrasonography (LUS) has been gaining wide consensus in clinical practice to successfully diagnose lung diseases.
Transient tachypnea of the newborn (TTN), first described by Avery and coworkers in 1966. The investigators named the disorder “Transient Tachypnea of the Newborn”(TTN) and speculated that it was the result of delayed clearance of fetal lung liquid. Risk factors for development of TTN include premature or elective cesarean delivery without labor, large birth weight, maternal diabetes, maternal asthma, twin pregnancy, and male gender [4]. Respiratory morbidity is inversely related to gestational age.
With the onset of labor, the pulmonary epithelium changes from a chloride-secreting membrane to a sodium-absorbing membrane, with reversal of the direction of flow of lung liquid. This change is an active metabolic process involving increased Na+K+ATPase activity in the epithelial cells and serves to drive liquid from the lung lumen into the interstitium [5]. In addition, because lung liquid contains very little protein, oncotic pressure also favors the movement of water from the air space back into the interstitium, and from there into the vascular compartment [6-8]. The mechanical force of birth canal squeeze was originally thought to be the major factor in lung fluid resorption but is now believed to be only a minor contributor [4]. Birth itself was shown to be associated with a surge in fetal catecholamine secretion, which was critically linked to an increase in β-adrenergic-stimulated lung liquid clearance by increased expression of ENaC and Na-K-ATPase activity [9]. A delay or impairment in lung fluid absorption at birth potentially leads to filling of the lung airspaces with fluid and causes a ventilation/perfusion mismatch, which eventually can culminate in transient tachypnea of the newborn (TTN) or neonatal respiratory distress syndrome (RDS). The diagnosis of transient tachypnea of the newborn (TTN) is traditionally based on clinical manifestations, arterial blood gas analysis (ABG) and chest x-ray (CXR). The radiographic features may occasionally look similar to pulmonary edema, meconium aspiration syndrome or RDS [10]. However, the use of this imaging technique is limited due to transportation issues and inevitable radiation. Ultrasound has been emerging to be useful in the diagnosis of TTN as well as prediction of the need for respiratory support in infants affected by TTN [11,12].
Terminology-
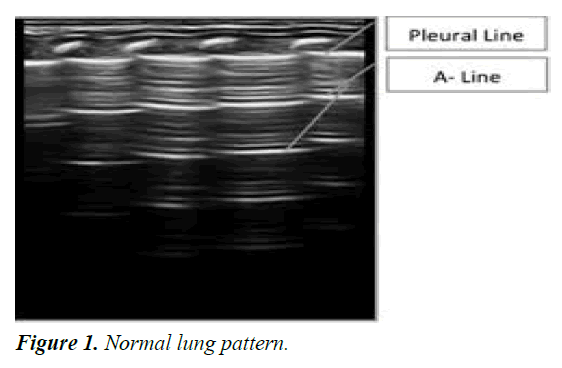
The normal lung is “black”. In a normally aerated lung, the only detectable structure is the pleura, visualized as a hyperechoic horizontal line. The pleural line moves synchronously with respiration [13]. This dynamic horizontal movement is called lung sliding.
Pleural line: It is a smooth regular hyperechoiec sliding line below the rib line usually measuring <0.5mm in thickness. Lung sliding is the movement of the pleura synchronized with respiration in a to-and-fro pattern [14].
A-line: These are hyperechoic, horizontal parallel lines arising at regular intervals from the pleural line. It arises from the reverberation artifact of the pleural line. The spacing of the A- line is equal to the distance between the pleural line and the skin [15] (Figure 1).
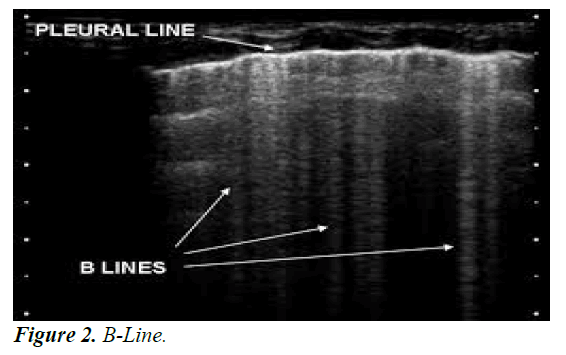
B line: B-lines are defined as discrete laser-like vertical hyperechoic reverberation artifacts that arise from the pleural line, extend to the bottom of the screen without fading, and move synchronously with lung sliding [16,17] their number increases along with decreasing air content and increase in lung density [18,19] (Figure 2).
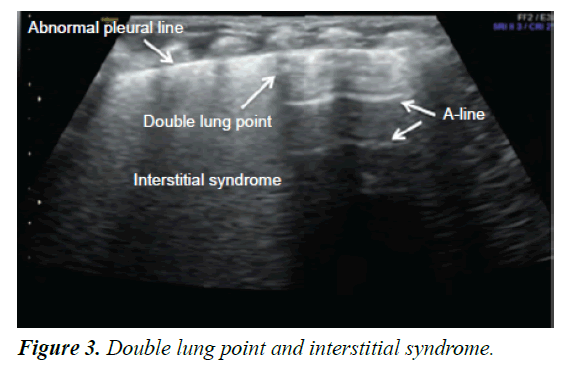
Double Lung Point (DLP): Because of a difference in the severity or nature of the pathological changes in different areas of the lung, a longitudinal scan shows a clear difference between the upper and lower lung fields; this sharp cutoff point between the upper and lower lung fields is known as the double lung ultrasound [20] (Figure 3).
Interstitial syndrome: The interstitial syndrome is the presence of areas of “white lung” or the presence of more than three B-lines in every examined area [21].
Bilateral “white lung”: Bilateral “white lung” is when compact B- lines appear in all 6 areas examined [21].
Materials and Methods
Source of data-
This is a descriptive study carried out on late preterm and term neonates in NICU, Department of Paediatrics, Kempegowda Institute of Medical Science, Bengaluru, Karnataka, India.
Inclusion criteria-
• Gestational age ≥ 34 weeks
• Symptoms of respiratory distress defined as:
- Tachypnea (respiratory rate >60 breaths per minute)
-Cyanosis (SpO2 <80%)
-Intercostal/subcostal retractions
-Grunting and/or nasal flaring
Exclusion criteria:-
• Neonates with prenatally diagnosed structural cardiac disease.
• Major multiple congenital anomalies.
• Other causes of respiratory distress like RDS, MAS, Congenital pneumonia, CNS insults etc.
Method of collection of data-
• Prior to conducting this study, we received informed consent from the neonate’s parents and approval from the Ethics committee of our hospital.
• All study subjects were selected from late preterm and term neonates admitted in neonatal intensive care unit of Kempegowda Institute of Medical Sciences, Bangalore and lung ultrasound was done at the earliest (<24 hours of birth) at bedside . Sixty five neonates were selected in the 18 months duration from January 2016 to June 2017 on the basis of clinical presentation.
• Detail history, clinical examination and necessary investigation was done.
Equipment used-
• GE Volusion 730 (GE Medical Systems, Milwaukee, USA) ultrasound instrument and a high definition linear array probe with a frequency of 11.0 MHz was used in this study.
Examination method-
• In a quiet state, the infants were placed in the supine, lateral, or prone position for the scan. Each lung was divided into 3 regions anterior, lateral, and posterior regions by the anterior and posterior axillary line.
• The ultrasound probe was placed perpendicular to the ribs. Each region of both lungs was carefully scanned and looked for the following observation indexes which include the normal pleural lines, A lines, Blines and double lung point (DLP).
Statistical Analysis
Data entry and data analysis-
Data was entered in Microsoft Excel spreadsheet. Data was analyzed in EpiData analysis software version 2.2.2.182 (EpiData Association, Odense, Denmark).
Categorical variables like gender, mode of delivery, gravida, clinical signs, USG findings were summarized as proportions. Continuous variables like age, heart rate, respiratory rate, nasal flaring, chest retractions and hospital stay were summarized as mean and standard deviation. Comparison of two categorical variables was done using Chi square test. A P value of less than 0.05 was considered as statistically significant.
Results
In our study, among 65 cases, mean age distribution of study participants (in hours) at which LUS was done is 8.9 hours.
The gender distribution of the study participants was 45 (69.2%) male infants and 20 (30.8%) female infants. Among the 65 babies enrolled, 45 (69.2%) babies were delivered to primi mothers. In this study, term babies were 41 (63.1%) while late preterm babies were 24 (36.9%) and 43 (66.2%) babies were delivered through LSCS. Out of 65 neonates in the study, babies with birth weight of >2.5 kg constituted 50 (76.9%) as most of them were term babies whereas babies with birth weight of 1-2.49 kg was 15 (23.1%) as shown in Table 1. The most prominent clinical feature in the study was tachypnea with 58 (89.2%) neonates having a respiratory rate of >60 while nasal flaring and intercostal retractions was observed in 29 (44.6%) neonates each. The respiratory symptoms subsided in 38 (58.4%) babies at room air while only 2 (3.1%) babies required nasal CPAP. On lung ultrasound, 53 (81.5%) neonates showed the feature of double lung point (DLP) while 41 (63.1%) neonates showed A-line. These LUS findings was compared with the gestational age, obstetric score, mode of delivery, gender of the babies, birth weight and the clinical findings to look for any statistical significance. The DLP feature on LUS was significantly more in babies born to primi mothers than in babies born multigravida (p value 0.02). The DLP point feature on LUS showed statistical significance among babies delivered through LSCS when compared to babies delivered vaginally (p value-0.01) (Table 2).
| Characteristics | Number (n) | Percentage (%) |
|---|---|---|
| Gender | ||
| Number | Male | Female |
| 45 | 69.2 | |
| Percentage | 20 | 30.8 |
| Obstetric score | ||
| Primigravida | 45 | 69.2 |
| Multigravida | 20 | 30.8 |
| Gestational age | ||
| Late preterm | 24 | 36.9 |
| Term | 41 | 63.1 |
| Mode of delivery | ||
| Vaginal delivery | 22 | 33.8 |
| LSCS | 43 | 66.2 |
| Birth weight | ||
| 1-2.49 | 15 | 23.1 |
| ≥2.5 | 50 | 76.9 |
Table 1. Characteristics of study subjects.
| Characteristics | Number/Percentage (%) | p-value (student T test) | |
|---|---|---|---|
| Gender | |||
| Male | Yes | 36 (67.9) | 0.63 |
| No | 9 (75) | ||
| Female | Yes | 17 (32.1) | |
| No | 3 (25) | ||
| Obstetric score | |||
| Primi | Yes | 40 (75.5) | 0.02* |
| No | 5 (41.7) | ||
| Multi | Yes | 13 (24.5) | |
| No | 7 (58.3) | ||
| Gestational age | |||
| 34-36 wk | Yes | 21 (39.6) | 0.34 |
| No | 3 (25) | ||
| >37 wk | Yes | 32 (60.4) | |
| No | 9 (75) | ||
| Mode of delivery | |||
| Normal | Yes | 7 (13.3) | 0.01* |
| No | 5 (41.7) | ||
| LSCS | Yes | 46 (86.7) | |
| No | 7 (58.3) | ||
| Birth weight | |||
| 1-2.49 kg | Yes | 12 (22.6) | 0.86 |
| No | 3 (25) | ||
| >2.5 kg | Yes | 41 (77.4) | |
| No | 9 (75) | ||
Table 2. Comparison of DLP with the mentioned characteristics.
On comparing the clinical features with DLP, nasal flaring (p value-0.02) and intercostal retractions (p value- 0.05) was statistically significant whereas SCR was not found to be significant (p value-0.89). The demographic variables on comparison with LUS indices of A-line and B-line did not show any statistical significance likewise the clinical findings of respiratory distress like nasal flaring and intercostal retractions was not statistically significant with the observation indexes of A-line and B-line.
Discussion
The incidence rates of TTN are from 4.0% to 5.7% among term infants and 10.0% among premature infants [22]. Though TTN is mostly a self-limiting condition, treatment is mainly supportive with provision of supplemental oxygen, as needed. More severe cases may respond to continuous positive airway pressure (CPAP) to improve lung recruitment.
Levine et al. [23] stated that respiratory conditions which prompt admission to the NICU (ie, persistent pulmonary hypertension and transient tachypnea) were almost threefold greater in the elective cesarean group than among vaginally delivered neonates. Our findings confirm this risk of TTN being significantly more in babies delivered via cesarean section. Tutdibi [24] indicates that TTN is strongly related to elective cesarean section and low GA.
Male sex was regarded as significant risk factor for respiratory distress (p-value.0.026) by Hameed et al. [25], and same finding was reported by Ingemarsson [26] and Rawlings [27] In our study, 40 babies born to primi mothers showed a statistical significance (p value-0.02) when compared to babies born to multi gravid mothers while Hameed et al. studied the respiratory distress (RD) in term infants, showed that RD was more in babies born to multigravidas but was not significant (p value-0.73). This aspect may require further evaluations.
According to Liu et al. [28], the main ultrasonic imaging features of TTN include DLP. The sensitivity and specificity of DLP for the diagnosis of TTN were 76.7% and 100% respectively. Similarly DLP was found in majority of our cases, 53 neonates constituting 81.3% of our study population. It is estimated that over 70% of infants with TTN are clinically misdiagnosed with RDS. Based on the previous literature reports [29-31], lung consolidation with air bronchograms without DLP was the primary ultrasonic feature of RDS, whereas DLP without lung consolidation was the most specific ultrasonic feature of TTN. In a prospective cohort study of 59 neonates with respiratory distress, Vergina et al. identified that the sensitivity and specificity of lung ultrasound for TTN were 93.3% and 96.5%, which were higher than 89.4% and 91.3% for X-ray, respectively. Thus, current evidence on lung ultrasound for the diagnosis of TTN is accurate and reliable [32,33].
Conclusion
In conclusion, the results of our study further demonstrate that LUS can accurately and reliably diagnose TTN. It has advantage that it cannot be duplicated by chest computed tomography or CXR examination. The lung ultrasound has many advantages. First, the ultrasound can be performed at the bedside, being non-ionising. Second, the ultrasound is easy to operate, and can be repeated several times a day without hazards to the operator or the patient. Third, this is a low-cost technique, which requires only elementary skills. Last but not least, the lung ultrasound has very high accuracy and reliability in diagnosing pulmonary disease. Given all of these, this method could replace radiography as the first-line diagnostic approach in neonatal period.
We acknowledge that our findings have limitations that restrict the immediate generalization of our results. We believe that investigating lung ultrasound changes in a neonate with respiratory distress is a clinically relevant topic for a separate study. We hope that this will help clinicians become acquainted with LUS and will accelerate the extensive application of LUS in children.
Acknowledgments
Dr. Sanjay SC, Associate Professor, Department of Radiodiagnosis, KIMS, Benguluru, Karnataka, India.
Dr. Janardhan P, Senior Resident, Department of Radiodiagnosis, KIMS, Benguluru, Karnataka, India.
References
- Chen SW, Zhang MY, Liu J. Application of lung ultrasonography in the diagnosis of childhood lung diseases. Chin Med J. 2015; 128: 2672-2678.
- Wardlaw T, Salama P, Johansson EW, et al. Pneumonia: The leading killer of children. Lancet. 2006; 368: 1048‑1050.
- Cloherty J, Eichenwald E, Hansen A. Transient of tacypnea of the newborn. Manual of Neonatal Care. 7th ed. Philadelphia: Wolters Kluwer. 2015; 403-405.
- Fanroff J, Martin R, Fanaroff A. Neonatal Respiratory Disorders. Fanaroff & Martin’s Neonatal-Perinatal medicine. 10th ed. Philadelphia, PA: Elsevier/Saunders. 2015; p. 1127.
- Avery Gleason C, Devaskar S, Avery M. Transient tacypnea of newborn. Avery’s diseases of the newborn. Philadelphia, PA. Elsevier/Saunders. 2012; 697.
- Bland RD. Lung liquid clearance before and after birth. Semin Perinatol. 1988; 12: 124.
- Berthiaume Y, Staub NC, Matthay MA. Beta-adrenergic agonists increase lung liquid clearance in anesthetized sheep. J Clin Invest. 1987; 79: 335.
- Bland RD, Nielson DW. Developmental changes in lung epithelial ion transport and liquid movement. Annu Rev Physiol. 1992; 54: 373.
- Katz C, Bentur L, Elias N. Clinical implication of lung fluid balance in the perinatal period. Journal of Perinatology. 2011; 31: 230-235.
- Newman B. Imaging of medical disease of the newborn lung. RCNA1999; 37: 1049-1065.
- Copetti R, Cattarossi L. The “double lung point”: an ultrasound sign diagnostic of transient tachypnea of the newborn. Neonatology. 2007; 91: 203.
- Corbett HJ, Humphrey GM. Pulmonary sequestration. Paediatr Respir Rev. 2004; 5: 59.
- Volpicelli G, Elbarbary M, Blaivas M, et al. International Liaison Committee on Lung Ultrasound (ILCLUS) for Interna tional Consensus Conference on Lung Ultrasound (ICC-LUS). International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012; 38: 577-591.
- Lichtenstein DA, Menu Y. A bedside ultrasound sign ruling out pneumothorax in the critically ill. Lung sliding. Chest. 1995; 108: 1345-1348.
- Lichtenstein DA, Mezière G, Lascols N, et al.Ultrasound diagnosis of occult pneumothorax. Crit Care Med. 2005; 33: 1231-1238.
- Dénier A. Ultrasound: Its application to diagnosis. Presse Med. 1946; 22: 307-308.
- Lichtenstein DA, Lascols N, Mezière G, et al. Ultrasound diagnosis of alveolar consolidation in the critically ill. Intensive Care Med. 2004; 30: 276-281.
- Gargani L, Picano E, Caramella D, et al. Lung water assessment by lung ultrasonography in intensive care: a pilot study. Intensive Care Med. 2013; 39: 74-84.
- Soldati G, Copetti R, Sher S. Sonographic interstitial syndrome: The sound of lung water. J Ultrasound Med. 2009; 28:163-174.
- Copetti R, Cattarossi L. The “double lung point”: an ultrasound sign diagnostic of transient tachypnea of the newborn. Neonatology. 2007; 91: 203.
- Copetti R, Cattarossi L, Macagno F, et al. Lung ultrasound in respiratory distress syndrome: A useful tool for early diagnosis. Neonatology. 2008; 94: 52-59.
- Greenough A. Transient tachypnea of the newborn. In: Greenough A, Milner AD, editors. Neonatal Respiratory Disorder. London: CRC Press. 2003; 272-277.
- Levine E, Ghai V, Barton J, et al. Mode of delivery and risk of respiratory diseases in newborns. Obstetrics and Gynecology. 2001; 97: 439-441.
- Tutdibi E, Gries K, Bucheler M, et al. impact of labor on outcomes in transient tachypnea of the newborn: Population-based study. Pediatrics. 2010; 125: e577-e583.
- Hameed N, Al-Janabi M, Al-Reda Y. Respiratory distress in full term newborns. The Iraqi Postgraduate Medical Journal. 2017; 6: 233-239.
- Ingemarrson I. Gender aspects of preterm birth. BJOG. 2003; 20: 3408.
- Rawlings JS, Smith FR. Transient tachypnea of newborn, an analysis of neonatal and obstetric risk factors. Am J Dis Child. 1984; 183: 869-871.
- Liu J, Wang Y, Fu W, et al. Diagnosis of neonatal transient tachypnea and its differentiation from respiratory distress syndrome using lung ultrasound. Medicine. 2014; 93: e197.
- Lichtenstein DA, Lascols N, Mezière G, et al. Ultrasound diagnosis of alveolar consolidation in the critically ill. Intensive Care Med. 2004; 30: 276-281.
- Lovrenski J. Lung ultrasonography of pulmonary complications in preterm infants with respiratory distress syndrome. Ups J Med Sci. 2012; 117: 10-17.
- Stefanidis K, Dimopoulos S, Tripodaki ES, et al.Lung sonography and recruitment in patients with early acute respiratory distress syndrome: A pilot study. Crit Care 2011; 15: R185.
- Vergine M, Copetti R, Brusa G, et al. Lung ultrasound accuracy in respiratory distress syndrome and transient tachypnea of the newborn. Neonatology 2014; 106: 87-93.
- Smith-Bindman R. Is computed tomography safe? N Engl J Med. 2010; 363: 1-4.