Current Pediatric Research
International Journal of Pediatrics
Correlation of upper limb coordination with fine motor precision, fine motor integration and manual dexterity in cerebral palsy children.
Shreya Shah1, Abhijit Satralkar2*
1Department of Physiotherapy, PES Modern College of Physiotherapy, Pune, India
2Department of Neurophysiotherapy, PES Modern College of Physiotherapy, Maharashtra University of Health Science (MUHS), Pune, India
- Corresponding Author:
- Abhijit Satralkar
Department of Neurophysiotherapy,
PES Modern College of Physiotherapy,
Maharashtra University of Health Science (MUHS),
Pune, India
E-mail: shah.shreya8632@gmail.com
Received: 27 March, 2023, Manuscript No. AAJCP-23-94839; Editor assigned: 29 March, 2023, Pre QC No. AAJCP-23-94839(PQ); Reviewed: 12 April, 2023, QC No. AAJCP-23-94839; Revised: 19 April, 2023, Manuscript No. AAJCP-23-94839(R); Published: 27 April, 2023, DOI:10.35841/0971-9032.27.04.1185-1189.
Aim: Cerebral palsy is a clinical manifestation of several cerebral cortical or subcortical injuries during the first year of life. Cerebral palsy is most likely in premature babies. Cerebral palsy affects posture and mobility. Prenatal brain injury causes it. Basic motor skills are essential for acquiring complicated motions and creating movements needed for sports that include object control (throwing or catching a ball) or fundamental actions like jumping (running jumping skipping) Early motor skill development is linked to physical, social, and cognitive development. Motor development has six phases: reflexive, preadapted, fundamental patterns, context-specific, skilled, and compensatory. Objective: To find out correlation between upper limb coordination with fine motor precision and fine motor integration, to find out correlation between manual dexterity with fine motor precision and integration and to find out correlation between manual coordination with fine manual control by using bruininks-osteretsky test. Methods: In this study 30 subjects diagnosed with cerebral palsy were selected. Motor integration, manual dexterity, and upper limb coordination were assessed in cerebral palsy patients by using bot toolkit. Tool kit tasks were used to evaluate fine manual control and coordination. Age-gender analysis determined the subject's point score and standard scoring. The subject was demonstrated and given three trials for the exercises, and the sums of motor proficiency, motor integration, manual dexterity, and upper limb coordination were recorded. Results: There was a positive correlation between upper limb coordination and fine motor precision, fine motor integrity, manual coordination, and fine manual control, based on the following data of children with cerebral palsy between the ages of 5 and 15 years. Conclusion: This study concludes that the bruininks-osteretsky toolkit has been an effective tool in children diagnosed with cerebral palsy and in improving motor activities.
Keywords
Cerebral palsy, Bruininks–osteretsky test, Fine motor activities, Manual control, Manual coordination.
Introduction
Control over objects (throwing or catching the ball), fundamental loco motor motions (running, jumping, skipping), and stability, i.e., balance, are all examples of basic motor skills that are essential for the development of more complex motor abilities [1] and for participation in sports. Early childhood is crucial for the maturation of motor abilities, which are linked to later health and well-being in terms of things like cardiorespiratory fitness and body fat percentage. In 1862, an orthopedic surgeon named William James Little initially described Cerebral Palsy (CP). Cerebral palsy is the clinical manifestation of a wide range of cerebral cortical or subcortical lesions occurring within the first year of life, despite its common perception as a movement condition caused by a nonprogressive (static) damage to the growing brain.
Infants born prematurely have the highest rate of cerebral palsy. Intra-Ventricular Haemorrhage (IVH) and periventricular leukomalacia are the most common CNS consequences of preterm, and they cause severe damage to the developing brain at a vulnerable time (PVL). Family-centered services that make a difference in the lives of children with cerebral palsy and their families are essential, as these kids face a wide range of challenges and, in some cases, disabilities. Cerebral Palsy (CP) in children can cause a wide range of motor deficits and functional restrictions [1]. Understanding how these factors are distributed among children with Cerebral palsy and how certain deficits relate to activity restrictions might inform rehabilitation objectives.
Accurate longitudinal research and health service planning can be facilitated by collecting quantitative data on motor deficits and activity restrictions in people with Cerebral palsy. Physical therapists' assessments of patients' motor performance during rehabilitation are an important source of evaluation and efficacy data. To help with initial treatment planning and give a thorough study of motor components linked to positive rehabilitation results [2,3], performance-based evaluations are performed with both children and adults. Especially now, when higher levels of competence and responsibility are required of everyone, the creation of a performance profile for children with mild motor impairments is a useful assessment guideline [4,5].
Bruininks-oseretsky test of motor proficiency
The bruininks-oseretsky test of motor proficiency was created to aid teachers, clinicians, and researchers in assessing kids motor skills, creating, and evaluating motor training programs, and identifying children with severe motor dysfunctions or developmental delays [6]. These kids might be labeled as having clumsy kid syndrome, sensory integration disorder, or developmental coordination disorder [7]. In 1972, Dr. Robert H. bruininks initiated work on what would become known as the bruininks-oseretsky test. Bruininks modelled his evaluation in part after the Americanized version of oseretsky's motor skills test. The new test contains some questions that are identical to those on the old test, but it also has significant improvements in terms of substance, structure, and technical aspects. This exam is a motor functioning evaluation for kids ages 4.5 to 14.5 and is done on an individual basis.
The whole battery consists of eight tests with a total of fortysix items, allowing for a detailed index of motor proficiency as well as individual assessments of both gross and fine motor skills. The whole battery consists of 28 things, however only the first 14 are included in this brief overview of motor skills. The latest generation of testing technology is developed with the goals of creating a positive testing environment for kids and teenagers, standardising the process, and streamlining the administration and scoring of tests. Each of the bruininks-eight oseretsky's subtests is tailored to evaluate a certain facet of motor growth. There are four subtests that assess one's large motor skills, three that assess one's small motor skills, and one that assesses both. Comparing performance in different domains is made possible through the distinct assessment of gross and fine motor skills [8].
Need of study
• Testing of motor performance during rehabilitation by
physical therapists is a significant source of evaluation and
efficacy data.
• In order to help direct initial treatment planning and offer a
full examination of motor components important to
successful rehabilitation, performance-based evaluations
are performed for both children and adults.
• Several standardized assessments of motor performance are
available to physical therapists for certain pediatric or adult
groups; however, none have been proved to be appropriate
for both gross motor and fine motor evaluation.
• The bruininks-oseretsky test of motor competence was
created to aid teachers, clinicians, and researchers in
assessing students' motor skills, creating, and evaluating
motor training programs, and diagnosing children with
severe motor dysfunctions and developmental delays.
• So, the purpose of the current investigation is to evaluate
the gross and fine motor components of motor proficiency
in children with cerebral palsy.
Outcome measures
Motor skill analysis was conducted using the bruininksoseretsky test of motor proficiency, second edition (BOT-2).
Fine motor precision:
• Colouring shape: Circle,
• Colouring shape: Star,
• Drawing lines through paths curved,
• Drawing lines through paths crooked,
• Connecting dots,
• Folding paper,
• Cutting out a circle.
Assessment criteria-1
There are rules to follow for both the circle and the star in terms of their fundamental form, line closures, edges, orientation, and overall size. Precision is prioritized over speed; therefore subsets are not timed.
Finer motor integration:
• Copying a circle,
• Copying a square,
• Copying overlapping circles,
• Copying a wavy line,
• Copying a triangle,
• Copying a diamond,
• Copying a star,
• Copying overlapping pencils.
Assessment criteria-2
Criteria for circles, squares, wavy lines, triangles, diamonds, and stars in terms of their basic geometry, line closures, edges, orientation, and overall size.
Manual dexterity:
• Making dots in circles,
• Transferring pennies,
• Placing pegs into a pegboard,
• Sorting cards,
• Stringing blocks.
Assessment criteria-3
The greatest possible performance on each item will be recorded as a score, and those scores will be added together to generate an overall manual dexterity subset score.
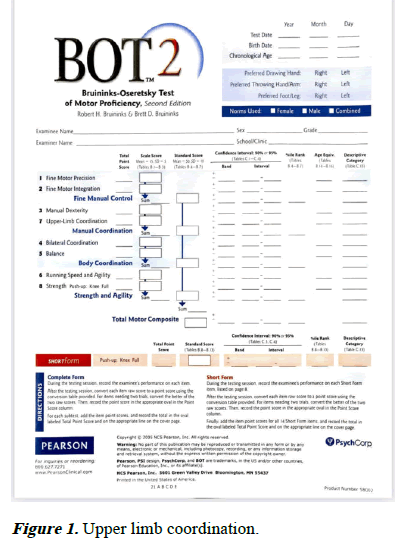
Upper limb coordination:
• Dropping and catching a ball both hands,
• Catching a tossed ball both hands,
• Dropping and catching a ball one hand,
• Catching a tossed ball one hand synchronized,
• Dribbling a ball one hand,
• Dribbling a ball alternating hands,
• Throwing a ball at a target (Figure 1).
Literature Review
A systematic analysis of research performed in healthy children, when children are physically active from a young age, they minimize their risk of developing a number of chronic diseases later in life, making motor skill competency a key indicator of health. The purpose of this research was to examine the validity of the shortened Bruininks-Oseretsky (BOT-2) in cross-sectional and post-test-only investigations among healthy youngsters. The PRISMA guidelines were followed throughout the search and analysis of the papers. 250 relevant studies published between 2011 and 2020 were found by a search of electronic databases (Google Scholar, PubMed, Mendeley, Science Direct, and Scopus). The quantitative synthesis included 21 studies with a total of 3893 male and female participants. As a result of this research, it is safe to say that the BOT-2 exam can be utilised to enhance motor proficiency in otherwise healthy youngsters. To this end, it is crucial to devote substantial resources to the development of various programs that help kids hone their motor skills and encourage them to experiment with new motions [9].
Materials and Methods
Materials and tools
• BOT-2 Tool kit,
• BOT-2 assessment form,
• Children’s shapes and toys,
• Pen,
• Paper.
Inclusion criteria:
• Children diagnosed with cerebral palsy of age group 5 to 15
years,
• Both males and females,
• Parents of children willing to participate,
• Baseline scores: The eligibility criteria will be dependent
upon the GMFC scale level 1 and above.
Exclusion criteria:
• Parents of children unwilling to participate,
• Children below 5 years of age,
• Auditory impairments,
• Cognitive impairments.
Results
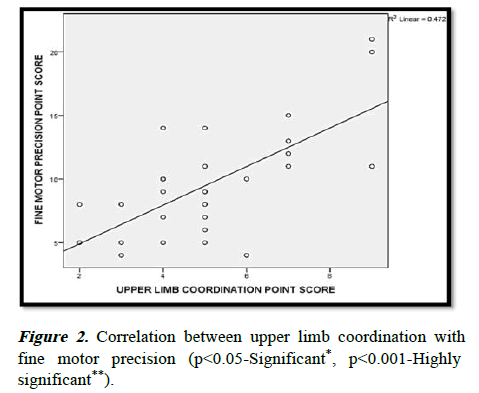
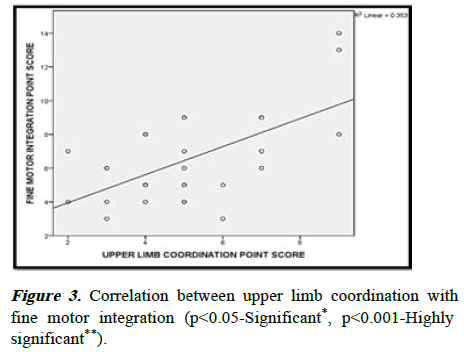
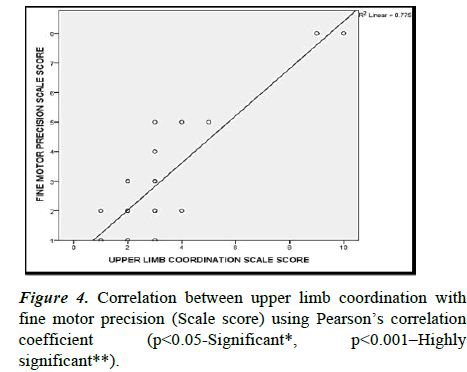
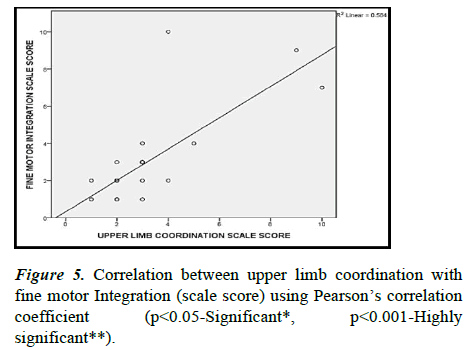
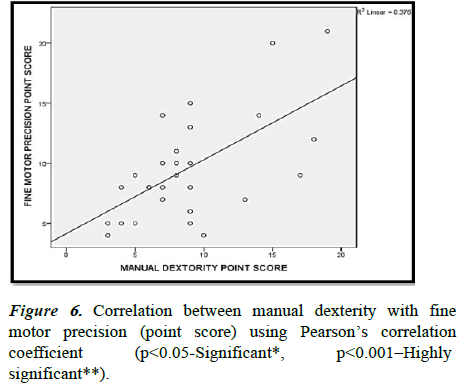
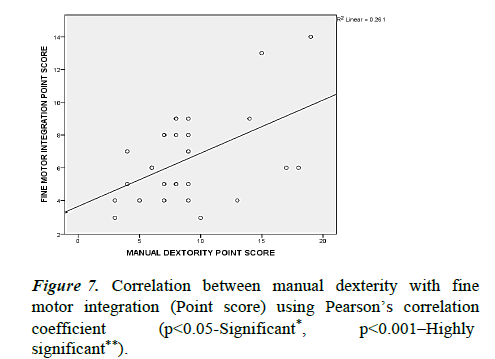
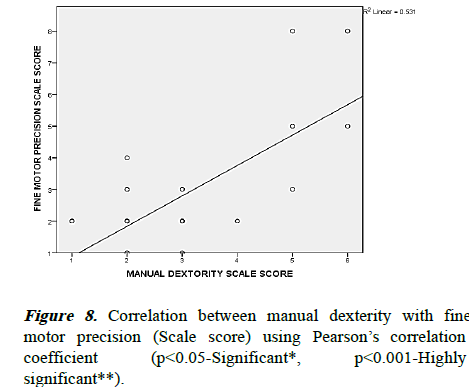
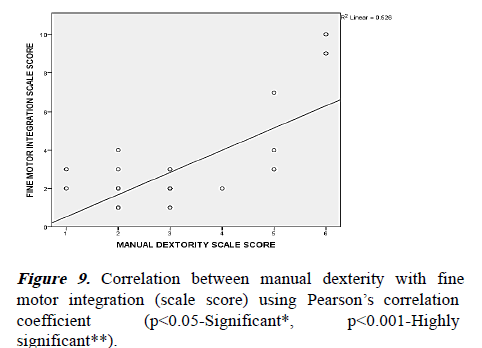
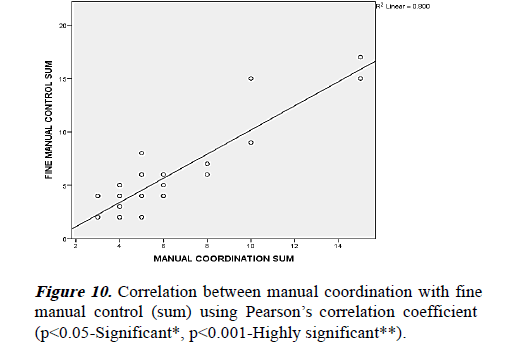
The following results from children with cerebral palsy between the ages of 5 and 15 show a positive relationship between upper limb coordination and fine motor precision, fine motor integrity, manual dexterity and fine motor precision and integration, and manual coordination and fine manual control (Tables 1-11). The BOT-2 can be used to evaluate the motor skills of anyone aged 5 to 15 (Figures 2-13) [10].
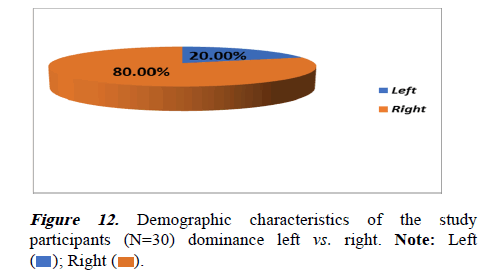
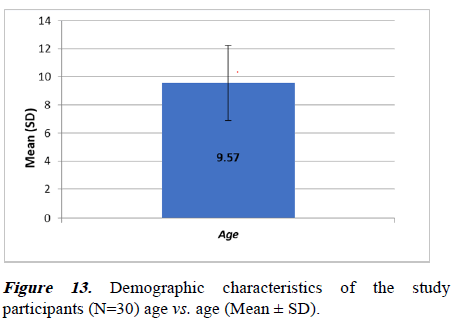
| Variables | Sub-groups | n | % |
|---|---|---|---|
| Gender | Male | 16 | 53.3 |
| Female | 14 | 46.7 | |
| Dominance | Left | 6 | 20 |
| Right | 24 | 80 | |
| Age (Mean ± SD) | 9.57 ± 2.674 | ||
Table 1. Demographic characteristics of the study participants (n=30).
| Variables | Mean | Standard deviation |
|---|---|---|
| Fine motor precision point score | 9.57 | 4.224 |
| Fine motor precision scale score | 2.77 | 1.813 |
| Fine motor integration point score | 6.5 | 2.675 |
| Fine motor integration scale score | 2.8 | 2.203 |
| Fine manual control sum | 5.53 | 3.857 |
| Manual dextority point score | 8.8 | 4.213 |
| Manual dextority scale score | 2.97 | 1.377 |
| Upper limb coordination point score | 5.07 | 1.911 |
| Upper limb coordination scale score | 2.93 | 1.999 |
| Manual coordination sum | 5.9 | 3.044 |
Table 2. Descriptive statistics (n=30).
| Mean ± SD | R-value | P-value | Result | |
|---|---|---|---|---|
| Upper limb coordination | 5.07 ± 1.991 | 0.687 | <0.001** | Positive |
| Fine motor precision | 9.57 ± 4.224 | |||
| Note:- **: Highly significant (p<0.001). | ||||
Table 3. Correlation between upper limb coordination with fine motor precision (point score) using Pearson’s correlation coefficient.
| Mean ± SD | R-value | P-value | Result | |
|---|---|---|---|---|
| Upper limb coordination | 5.07 ± 1.991 | 0.594 | <0.001** | Positive |
| Fine motor Integration | 6.50 ± 2.675 | |||
| Note:- **: Highly significant (p<0.001). | ||||
Table 4. Correlation between upper limb coordination with fine motor integration (point score) using Pearson’s correlation coefficient.
| Mean ± SD | R-value | P-value | Result | |
|---|---|---|---|---|
| Upper limb coordination | 2.93 ± 1.999 | 0.88 | <0.001** | Positive |
| Fine motor precision | 2.77 ± 1.813 | |||
| Note: **: Highly significant (p<0.001). | ||||
Table 5. Correlation between upper limb coordination with fine motor precision (scale score) using Pearson’s correlation coefficient.
| Mean ± SD | R-value | P-value | Result | |
|---|---|---|---|---|
| Upper limb coordination | 2.93 ± 1.999 | 0.764 | <0.001** | Positive |
| Fine motor integration | 2.80 ± 2.203 | |||
| Note:- **: Highly significant (p<0.001). | ||||
Table 6. Correlation between upper limb coordination with fine motor integration (scale score) using Pearson’s correlation coefficient.
| Mean ± SD | R-value | P-value | Result | |
|---|---|---|---|---|
| Manual dexterity | 8.80 ± 4.213 | 0.613 | <0.001** | Positive |
| Fine motor precision | 9.57 ± 4.224 | |||
| Note:- **: Highly significant (p<0.001). | ||||
Table 7. Correlation between manual dexterity with fine motor precision (point score) using Pearson’s correlation coefficient.
| Mean ± SD | R-value | P-value | Result | |
|---|---|---|---|---|
| Manual dexterity | 8.80 ± 4.213 | 0.511 | <0.001** | Positive |
| Fine motor integration | 6.50 ± 2.675 | |||
| Note:- **: Highly significant (p<0.001). | ||||
Table 8. Correlation between manual dexterity with fine motor integration (point score) using Pearson’s correlation coefficient.
| Mean ± SD | R-value | P-value | Result | |
|---|---|---|---|---|
| Manual dexterity | 2.97 ± 1.377 | 0.729 | <0.001** | Positive |
| Fine motor precision | 2.77 ± 1.813 | |||
| Note:- **: Highly significant (p<0.001). | ||||
Table 9. Correlation between manual dexterity with fine motor precision (scale score) using Pearson’s correlation coefficient.
| Mean ± SD | R-value | P-value | Result | |
|---|---|---|---|---|
| Manual dexterity | 2.97 ± 1.377 | 0.725 | <0.001** | Positive |
| Fine motor integration | 2.80 ± 2.203 | |||
| Note:- **: Highly significant (p<0.001). | ||||
Table 10. Correlation between manual dexterity with fine motor integration (scale score) using Pearson’s correlation coefficient.
| Mean ± SD | R-value | P-value | Result | |
|---|---|---|---|---|
| Manual coordination (sum) | 5.90 ± 3.044 | 0.895 | <0.001** | Positive |
| Fine manual control | 5.53 ± 3.857 | |||
| Note:- **: Highly significant (p<0.001). | ||||
Table 11. Correlation between manual coordination with fine manual control (sum) using Pearson’s correlation coefficient.
Discussion
The purpose of this research is to establish a connection between manual dexterity, manual coordination, and fine manual control, as well as between upper limb coordination, motor accuracy, and fine motor integration. Eight distinct assessments assess both fine and gross motor abilities. Fine motor competence includes abilities like manual dexterity, manual precision (the ability to control one's fingers and hands precisely), and fine motor integration (the ability to control one's fingers and hands precisely while also integrating visual cues with motor control) (e.g., Reaching, grasping and bimanual coordination with small objects). Coordination of the arms and hands is an example of gross motor competence (e.g., Visual tracking with coordinated arm and hand movement) girls and boys tend to fare differently on various subtests, therefore it's important to use sex and age-specific norms when interpreting test outcomes [10].
Scale scores were derived from the total number of points obtained on the subtests, whereas standard scores were utilized to evaluate motor composites. The overall motor composite score was calculated by adding the standard scores for the various motor composites together. Motor skill competency is a predictor of health since childhood physical activity reduces the risk of developing chronic diseases in later life. This analysis of BOT-2 studies in healthy youngsters aimed to establish its prospective and cross-sectional value. The search and analysis were conducted using PRISMA criteria. Google Scholar, PubMed, Mendeley, Science Direct, and Scopus yielded 250 studies from 2011-2020. This quantitative review of the literature includes 21 researches, totaling 3893 participants [11].
Conclusion
The study concludes that there is a positive correlation of upper limb coordination with fine motor precision, fine motor integration and manual dexterity in cerebral palsy children when compared to their motor activities using BOT-2 tool set. Given the children's ability to complete the tasks in the allotted time, their performance may be used as a benchmark against which the motor skills of other children can be compared. This study demonstrated the BOT-2 test's generalizability, showing that it can enhance children's motor skills that are otherwise healthy. Kids can develop better motor skills and expand their range of motion if they engage in a wide variety of activities over a long period of time. To examine the differences in motor function between male and female children with cerebral palsy, the BOT-2 set of instruments was used. Given the children's ability to accomplish the tasks in the allocated time, their performance may be used as a standard against which the motor skills of other children may be compared.
Declaration by Authors
Acknowledgement
None
Conflict of interest
The authors declare no conflict of interest.
Source of funding
None
Ethical approval
Approved
 Female
Female  .
.