Current Pediatric Research
International Journal of Pediatrics
A study of clinical profile of Multi Inflammatory Syndrome Child (MIS-C) patients from 1 month to 12 years admitted to paediatric ward in a tertiary care centre in Western Maharashtra.
Shraddha Laxman Khalate*, Sudhir Sarawade, Vijaylaxmi Sharma and Pallavi Kharade
Department of Pediatrics, RCSM GMC Kolhapur, Maharashtra, India
- Corresponding Author:
- Dr Shraddha Laxman Department of Pediatrics ,RCSM GMC Kolhapur , Maharashtra , India E-mail: kshraddha08@yahoo.co.in
Received: 11 April, 2022, Manuscript No. AAJCP-22-56989; Editor assigned: 14 April, 2022, PreQC No. AAJCP-22-56989 (PQ); Reviewed: 28 April, 2022, QC No. AAJCP-22-56989; Revised:12 May, 2022, Manuscript No. AAJCP-22-56989(R); Published: 26 May 2022, DOI:10.35841/0971-9032.26.5.1346-1350.
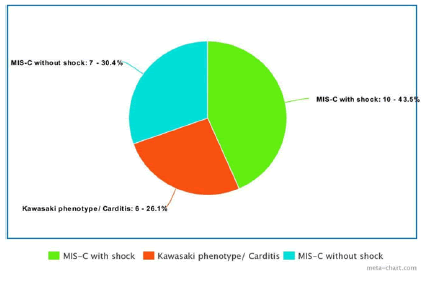
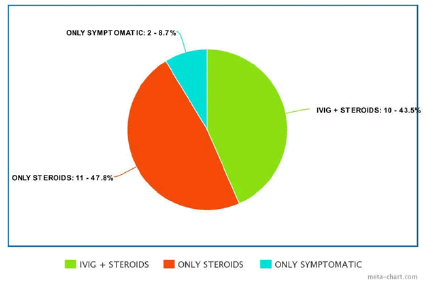
Background: Multisystem Inflammatory Syndrome-Child (MIS-C) is a rare but life-threatening complication of COVID-19 in children. Objective: To study clinical profile of patients with MIS-C in pediatric ward in a tertiary care centre in Western Maharashtra Study design: Observational study Participants: Patients satisfying MIS-C criteria by WHO during the study period Results: 3.1 % (23 cases) of the total admissions during the study period in the pediatric ward were cases of MIS-C. The median age of MIS-C cases was 5 years (1.5 months to 12 years). Out of 23 cases, 10 cases were with shock, 7 cases without shock and 6 cases were of Kawasaki phenotype. They were treated with steroids alone, steroids plus IVIG or only symptomatic treatment. There was mortality in 1 patient (4.3%). Conclusion: Steroids and IVIG can be lifesaving in MIS-C cases if diagnosed early and given prompt treatment.
Keywords
WHO criteria, Kawasaki phenotype, IVIG, steroids.
Introduction
Multisystem Inflammatory Syndrome in Children (MIS-C) is associated with recent or current SARS-CoV-2 infection. In children, COVID-19 is usually mild. However, in rare cases, children can be severely affected, and clinical manifestations may differ from adults.
In April of 2020, reports from the United Kingdom documented a presentation in children similar to incomplete Kawasaki Disease (KD) or toxic shock syndrome [1,2].
Since then, there have been reports of similarly affected children in other parts of the world. The condition has been termed multisystem inflammatory syndrome in children (MISC; also referred to as Pediatric Multisystem Inflammatory Syndrome (PMIS), Pediatric Inflammatory Multisystem Syndrome Temporally associated with SARS-CoV-2 (PIMSTS), pediatric hyper inflammatory syndrome, or pediatric hyper inflammatory shock).
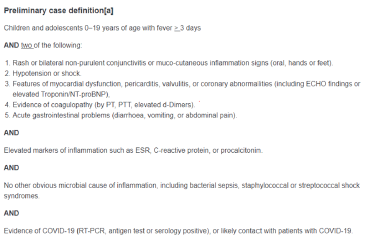
WHO has defined MIS-C on the basis of following criteria 3 as follows? (Figure 1).
Materials and Methods
This study was undertaken in pediatric ward in a tertiary care centre in Western Maharashtra from the month of June 2021 to Dec 2021. Clearance from ethical committee was achieved. WHO criteria were used for the inclusion of study cases [3].
Aim
To study clinical profile of Multi-Inflammatory Syndrome- Child (MIS-C) from 1 month to 12 years admitted in pediatric ward in a tertiary care centre in Western Maharashtra.
Objectives
• To study various demographic features and clinical presentation in children with Multi-Inflammatory Syndrome-Child (MIS-C).
• To find the percentage of MIS-C patients in total admissions from June 21 to December 21 at our centre.
• To assess the severity and outcome of the MIS-C patients admitted in our centre.
Inclusion criteria
All patients with a positive serology for SARS-CoV2 (RTPCR/ serology) and symptoms, signs, and laboratory markers in favor of a systemic hyper inflammatory condition, fulfilling the WHO criteria for MIS-C.
Exclusion criteria
Those with proven infective causes like dengue, leptospirosis and bacterial sepsis were excluded by appropriate investigations. COVID-19 RTPCR was done in all patients.
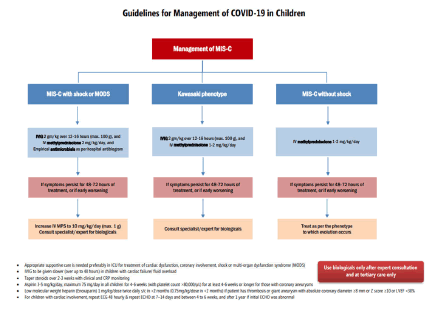
MOHFW (Ministry of Health and Family Welfare) guidelines were used for management of such cases [4] (Figure 2).
COVID-19 antibody testing was done using ELFA (enzyme linked fluorescent assay). Tier 1 investigations (CRP, ESR, serum albumin, LFT, RFT, serology for SARS-CoV2 and RTPCR swab for SARS-CoV2) were sent in all cases. 2 d echo was done in those having Kawasaki phenotype, cardiac involvement in form of carditis, arrhythmias and all those who presented with shock. Repeat 2 d echo on day 7 was done in all cases with Kawasaki phenotype.
Empirical antibiotics were started in all cases. Patients were categorized as MIS-C with shock, Kawasaki phenotype and MIS-C without shock. Clinical outcome and management were observed and studied.
Statistical Analysis
Data was entered in MS Excel and analyzed using SPSS 20. The results were expressed as mean ± SD for parametric data and median for non-parameteric data. Z-score of coronary artery diameter with value more than 2 were considered to have coronary artery dilatation/aneurysm [5].
Coronary artery changes like increased echogenicity and non-tapering in the absence of Z- score more than 2 were taken as non-specific coronary artery changes. Shock was defined when a patient required more than 20 ml/kg of IV fluid resuscitation or inotropic support to maintain blood pressure above the 5th centile.
Results
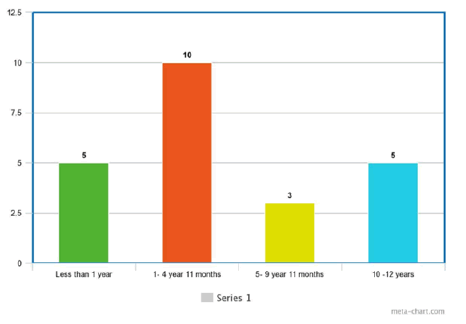
Out of 728 admissions from the month of June 2021 to December 2021, in our pediatric ward, 23 patients were diagnosed as MIS-C (3.1%). Out of 23, 11 were male and 12 were female (Figure 3).
The median age was 5 years (range 1 month to 12 years). Youngest age of presentation was 1.5 months the age distribution was as Figure 3. 11 cases were from urban areas, 12 were from rural areas. Out of 23, 2 patients were RTPCR swab positive (8.69%) and rest 21 had COVID-19 IG G antibodies positive (91.31%). 2 patients had documented past h/o.
COVID themselves (RTPCR positive) approximately 1.5 months prior to presentation. 2 patients had history of contact with COVID positive patients approximately 2 months prior. 4 patients had comorbidities (3 were cerebral palsy with global developmental delay, 1 was case of epilepsy).
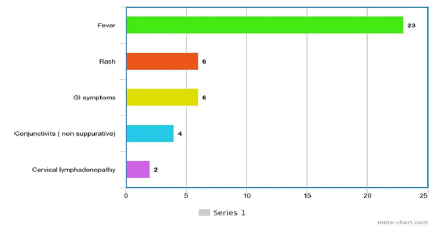
Fever was present in all 23 cases (100%). Rash was present only in 6 cases. Non suppurative conjunctivitis was present only in 4 cases. Gastrointestinal symptoms (abdominal pain/ diarrhea) were present in 6 cases. Cervical lymphadenopathy was present in 2 cases. Signs of shock were present in 10 cases. Cardiac involvement in the form of arrhythmias/signs of myocarditis/ECG changes was present in 6 cases. 5 cases presented with respiratory complaints such as cough and breathing difficulty. 2 cases had CNS symptoms in the form of seizures (Figures 4 and 5).
A study of clinical profile of Multi Inflammatory Syndrome Child (MIS-C) patients from 1 month to 12 years admitted to paediatric ward in a tertiary care centre in Western Maharashtra.
In the laboratory findings, absolute lymphocyte count was less than 1000 in 10 cases. ESR was raised >40 mm/hr in 15 cases. Thrombocytopenia (less than 1.5 lakh /cumm) was present in 8 cases. Low serum albumin (less than 2.5 g/dl) was present in 5 cases. Serum ferritin was raised, and CRP (>5 mg /dl) was positive in all 23 cases. D-dimer was positive in 20 cases (Figure 6).
All the patients were categorized as MIS- C with shock (10), MIS-C without shock (7), and Kawasaki phenotype (6). The average age of patients with shock was 7.025 years and patients without shock were 4.08 years.
Inotropic support was given to all 10 patients with shock in the form of inj adrenaline . Oxygen support was given to all patients presenting with shock in the form of nasal prongs approximately 4 L/min for initial few days. 2 patients were given oxygen by non- rebreathing mask with reservoir. 1 patient required invasive mechanical ventilation.
Steroids in the dose of inj methyl prednisolone (2 mkd) were given to all patients with shock. 6 patients even required dose to be escalated to 10 mkd. 5 patients without shock were given inj methyl prednisolone in dose of 1 mkd in view of persistent fever and raised inflammatory markers. Steroids were given intravenously over 5 days and then gradually tapered over 2-3 weeks by oral route. 2 patients without shock did not require steroids at all and they resolved spontaneously. Average duration of resolution of fever was 2.5 (range 1.5-4.5) days after receiving of steroids (Figure 7).
IVIG was given in 10 patients (6 with Kawasaki disease and 4 with steroid and inotropic resistant shock). 1 patient of Kawasaki phenotype required repeat dose of IVIG in view of persistent symptoms myocarditis. None of the cases were given biological agents.
There was death of patient with shock (11 months old), who had comorbidity of cerebral palsy with seizure disorder with global developmental delay with severe acute malnutrition. She presented as a diagnosed case of MIS-C, referred from peripheral centre, with refractory shock, required mechanical invasive ventilation at the time of admission itself and succumbed before she could receive IVIG. The average duration of stay was 10.75 in remaining 22 cases.
MIS-C with shock
• Total 10 out of 23 cases
• 7 were referred from peripheral centres
• All were given empirical antibiotics and oxygen support
• All were given inotropic support-inj adrenaline (1:10000)
• All were given inj methyl prednisolone 10 mkd in 4 patients and 20 mkd in 6 patients
• IVIG (2 gm/kg) was given in 4 patients with refractory shock. 1 patient required second dose of IVIG in view of no improvement.
• No case was given biological (tocilizumab/infliximab).
• There was death of 1 patient
Kawasaki phenotype
• Total 6 out of 23 cases
• Featuresofmyocarditis/arrhythmias/ECGchanges/ cardiacfailure/rashwere present at the time of presentation
• NT pro BNP was raised in all 6 cases
• 2 D ECHO was done in all these cases
• 4 patients had coronary artery involvement with z score >3.5
• All were given IvIg 2 gm/kg with Inj methyl prednisolone (2 mkd )
• Enoxaparin (1 mkd sc) was given to 2 patients with signs of cardiac failure and coronary root dilatation
• Tab aspirin was given by 5 mkd to all 6 cases and advised to continue for 4 weeks.
• 2d echo was repeated on day 7 for all patients and were advised follow up 2 decho after 4 weeks
• Resolution was seen in 5 out of 6 cases in review 2 d echo
Discussion
The first published study of multisystem inflammatory syndrome in children (MIS-C) described 8 children from the United Kingdom with hyper inflammatory shock 1; since then, several additional descriptive studies have contributed a wider breadth of knowledge about the clinical picture for the syndrome, now referred to as MIS-C.
Due to asymptomatic nature of COVID presentation in pediatric patients, most pediatric COVID cases go unnoticed. Hence if they present as post COVID hyper inflammation, history of COVID is difficult to illicit. IG G COVID antibodies titre can be helpful in such cases. Strong suspicion is needed in cases of fever without focus. Characteristic features such as rash, non-suppurative conjunctivitis, shock can help in diagnosis. Laboratory markers aid in further evaluation.
Early intervention for shock, using appropriate dose of methyl prednisolone and IVIG wherever needed, can be lifesaving. IVIG may not be needed in all cases of shock; few respond to only steroids too, similar conclusions were drawn from study in Kerala [6]. Few cases in our study that did not have shock (febrile inflammatory syndrome) and milder symptoms did not even require steroids and they resolved spontaneously.
Percentage of coronary artery aneurysm (1 in 12) was similar to another study in USA [7]. Mortality of 4.3% is similar to a study in Mumbai which also observed that 65% patients presented in shock; these children had a higher age (P=0.05), and significantly higher incidence of myocarditis with elevated troponin, NT pro BNP and left ventricular dysfunction, along with significant neutrophilia and lymphopenia, as compared to those without shock [8].
CNS symptoms and respiratory symptoms were comparatively lower in our study unlike a study in Northern India. Unusual neurological manifestations were found in a study of 21 MIS-C cases in northern India. They found predominant clinical manifestation as fever (100%), neurological manifestations (80%), lower respiratory tract infection (50%), rash (35%) and acute gastroenteritis (25%) [9].
A study in Cape Town, South Africa found that out of 23 patients of MIS-C, all 23 had required IVIG administration with 0% mortality [10]. We also found that dengue fever with shock was the closest differential diagnosis to MIS-C. Few patients referred from peripheral centres as MIS-C were later on diagnosed as dengue fever on investigations. Observational nature of study and limited matching cohorts were the limitations of the study. Larger data is required to apply statistical tests. Long term outcomes of MIS-C need to be studied further.
Conclusion
MIS-C is a life threatening COVID complication which can be attended by prompt suspicion and timely interventions. Substantial number of cases can be managed alone by intravenous steroids alone in a resource limited setting. Need of anticoagulants is lesser in pediatric population as compared to adults.