Current Pediatric Research
International Journal of Pediatrics
One stitch abdominal closure herniotomy: An alternative to Laparoscopic hernia repair in infants.
Married Doctors Hostel, Srinager, Jammu and Kashmir, India.
- *Corresponding Author:
- Raashid Hamid
Married Doctors Hostel
A-Block Room Number S-2
skims soura, Srinagar, Jammu and Kashmir
190011, India.
Tel: 09469451875
E-mail: drraashidhamid@gmail.com
Accepted date: November 30, 2016
Aim: To evaluate the feasibility of one-stitch herniotomy in the management of inguinal hernia in infants. Materials and methods: Between January 2011 and June 2014, 100 children in the age group 0–14 months with unilateral inguinal hernia were prospectively enrolled for hernia repair and herniotomy was performed by one-stitch technique. The primary outcomes were the time in the operating room and cosmesis. The secondary outcomes were postoperative pain and surgical complications. Results: Of the 100 children who were included in the study, 88 were males (male/female ratio 7.3:1). The mean operating time was 14.99 ± 2.69 min with a total mean time in the operating room was 38.23 ± 9.84 min. Postoperative analgesia was required in 16% infants with only 6% requiring two or more doses over 24 h period. There were no recurrent hernias with minimal postoperative complications on follow-up. Contralateral metachronous inguinal hernia was seen in 10% children on follow-up. Cosmesis was excellent with overall reduced total procedure costs. Conclusion: One-stitch herniotomy is an excellent alternative to both conventional and laparoscopic hernia repair in children requiring less expertise and logistics with overall reduced procedure costs. Outcome in terms of cosmesis is excellent with minimal risks and complications.
Keywords
Complications, Infants, Inguinal hernia, One-stitch herniotomy.
Introduction
The hernias need to be addressed at an earlier stage to prevent the development of complications mainly strangulation. The risk of complications is more in children <6 months of age. About 90% of complications can be prevented if a hernia repair is performed within a month of diagnosis [1,2]. Almost all hernias in children are indirect type, where the gut or the omentum enters the preformed sac (patent processus vaginalis) deep inguinal ring and traverses the inguinal canal to reach the superficial ring. In the newborn, the length of inguinal canal is negligible. The rings are superimposed over each other and the hernia is anatomically lateral to the inferior epigastria vessels. Herniotomy is considered sufficient in infants and no repair or reinforcement of the inguinal canal is required. Traditionally, the method of herniotomy involves “the spermatic cord outside the superficial inguinal ring” approach. A skin crease incision about 2 to 3 cm long is made above the pubic tubercle. The incision is advanced, the inguinal canal is approached, and the procedure is completed. We present a series of cases where an incision 1 cm is made to approach the inguinal canal, herniotomy performed, and the incision closed with a single U-stitch.
The original technique of hernia repair as described by Ferguson et al. [3] is based on the standard principles of external oblique muscle, exposure of the internal ring, exposure of the sac, and the repair of the anterior wall of the inguinal canal. However, there has been a great variability in the technique of herniotomy among the pediatric surgeons over the past six decades as has been described by Levitt et al. [4].
Purpose of Study
The purpose of the study was to evaluate the feasibility, outcome and cosmesis of this novel method of one stitch abdominal closure technique of herniotomy
Methods
This was an interventional prospective study involving infants who underwent no stitch herniotomy for unilateral inguinal hernia between January 2011 and June 2013. A proper informed consent was obtained from the patients parents. Ethical permission was sought from hospital ethical committee. This study was conducted in the department of pediatric and neonatal surgery at our state hospital, which is a tertiary care hospital with all surgical super-specialties. Our department of pediatric and neonatal surgery performs about 180-200 surgeries per month. This procedure was conducted by a single surgeon, who has prior experience of more than 8 years in this field and holds a super spatiality (post doctoral degree) in pediatric and neonatal surgery recognized by the Medical council of India. The primary outcomes measured were the time in the Operating Room (OR), operating time, cosmesis and cost inputs. The secondary outcomes measured were postoperative analgesic requirement and surgical complications.
The study included 100 infants with unilateral inguinal hernias, of which 88 were males. Random sampling technique was used for patient selection. Data was recorded in the case files by the corresponding author. The data was analyzed stastically by SPSS software. Exclusion criteria were; 1) abdominal/pelvic/inguinal surgeries, 2) undescended testis, 3) obstructed/strangulated hernias, 4) bilateral inguinal hernias. Inclusion criteria were; 1) unilateral inguinal hernias, 2) Uncomplicated inguinal hernia, 3) age less than or equal to 12 months. All the clinical characteristics included birth weight, age and weight at the time of surgery, any co- morbidity, any associated congenital anomaly.
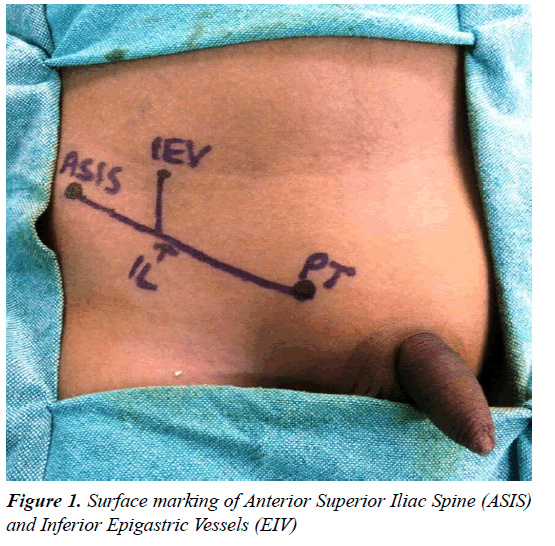
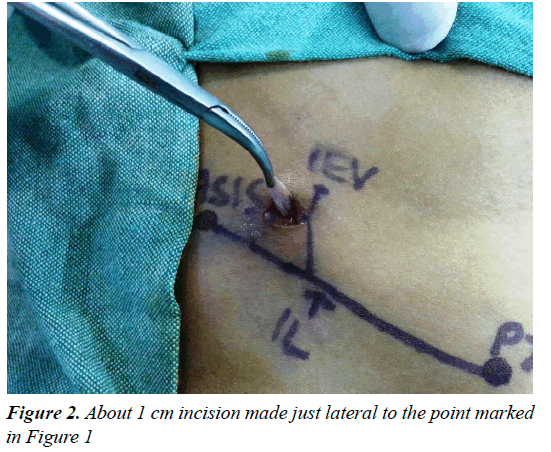
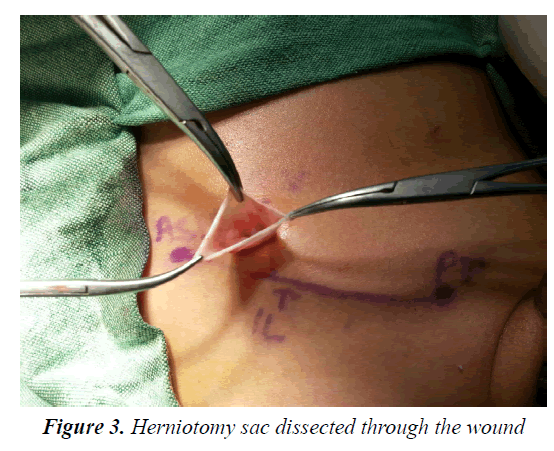
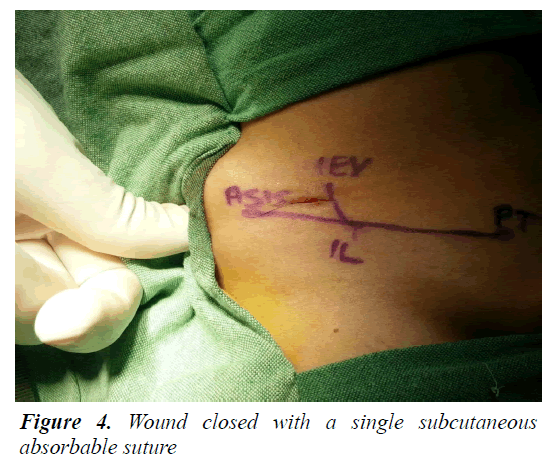
Patients were admitted on the day of surgery and were advised nil per os 4–6 h before the planned time of surgery. Procedure was performed under general anesthesia using laryngeal mask airway. Caudal analgesia using 0.2% ropivacaine 1 ml/kg was given to all patients. Patients were prepped and draped. Instruments required for this procedure includes few clips, two forceps, a scissor and an electric diathermy. Just above the mid-inguinal point, the pulsations of the inferior epigastric artery were felt and the point was marked (Figure 1). A 1 cm incision was made just lateral to this point (Figure 2). The external oblique aponeurosis is opened in the same line. The internal oblique muscle is split at its junction with the cremaster muscle. Sac is exposed, cord structures are lifted, and herniotomy is performed. A single U-stitch vicryl 4-0 is used to approximate the external oblique and the membranous layer of the superficial fascia and the subcutaneous tissue. Skin is not sutured but is approximated with sterile dressing (Figures 3 and 4).
The operating time was noted from making an incision till the closure of incision. The duration of the OR stay was calculated from the time of induction to complete arousal and shifting to recovery.
Patients received rescue analgesia in form of paracetamol rectal suppository (20 mg/kg) on need basis, which was subjective based on the mothers’ assessment of pain. The parents were asked to record the total number of analgesic doses required during the hospital stay and over the next 48 h. Most of the patients were observed for 6 h and were discharged after they had tolerated orals. Wound was kept open after first 24 h. All the preterm neonates were kept for an overnight hospital stay for observation to monitor apnea. Patients were followed at 3 days, 10 days, 6 months, 1 year and 2 years after the study for any postsurgical complications. The immediate postsurgical complications such as vomiting, transient voiding difficulty, wound infection, and hematoma formation were noted. Longterm complications such as contra lateral hernias, testicular atrophy (a decrease in the size of testis along long axis by more than 20% was considered significant), post-herniotomy hydrocele, and recurrent hernia were also recorded on follow-up. Average cost of this technique was 30 dollars (1800 Rupees).
Cosmetic results were scored by the operating surgeon and by an independent observer surgeon who was not performing the same procedure: bad/unsatisfactory=0, acceptable=1, good=2 and excellent=3.
Results
From January 2012 to June 2014, one-stitch herniotomy was performed on 100 successive infants with unilateral hernias. There were 88 males and 12 females (male/ female ratio 8.8:1). The age ranged from 11 days to 14 months with the mean age of 5 months. All the patients had unilateral hernias (right sided n=64; left sided n=36). The mean weight was 6.53 ± 1.604 kg.
The mean surgery time was 14.99 ± 2.69 min and the mean time spent in the OR was 38.23 ± 9.84 min. Of the 100 patients, 3 (3%) had prolonged stay in the OR with OR times being 78, 83 and 90 min, respectively. All of these were neonates and were born preterm. Of the 100 patients, 95 (95%) were discharged from the hospital 6 hours after the procedure and 5(5%) (All preterm neonates) were kept for overnight observational hospital stay. One of the neonates developed apnea and had to be mechanically ventilated overnight and was discharged after 36 h.
Of the 100 patients, 8 (8%) required a single dose of rescue analgesia (paracetamol suppository 20 mg/kg) during the 6 h of the hospital stay, 10 (10%) required a single analgesic dose, and 6 (6%) required two doses over the 24 h period. None of the patients required analgesics 24 h after the surgery. Transient voiding difficulty was seen in 7 (7%) infants and 3 (3%) experienced vomiting. None of our babies developed wound infection.
Of the 100 patients, 37 (37%) were followed for 2 years, 41 (41%) for 1 year and 22 (22%) for 6 months. There were no recurrences. One patient had a post-herniotomy hydrocele. A groin ultrasound ruled out a recurrence. The patient was managed and reoperated via scrotal approach for the hydrocele. None of the male patients had testicular atrophy on follow-up. Contralateral hernias were seen in 12 (12%) patients, (7 males and 5 females), on follow-up. Cosmesis was rated excellent in 98% patients and good in 2%. The mean cosmetic score was 2.98, which was excellent.
Discussion
Laparoscopic hernia repair is an established technique in adults [5]. Only a few studies have compared open and laparoscopic procedures of hernia repair in pediatric age group. The medical facilities and monetary affluence are unevenly distributed in rural and urban areas in developing countries. Hence, the need is to find the suitable treatment that is both scientifically/ethically correct while being cost effective [6]. Laparoscopic herniotomy is, no doubt, novel, safe, elegant and in some situations advantageous too. But the cost of setting up and running it may make it an unviable option in rural settings, where the majority of the developing world resides [7]. In a systematic review by Esposito et al, it seems that laproscopic herniotomy is faster than open herniotomy for bilateral hernias, whereas there is no significant difference in terms of operative time for unilateral inguinal hernia repair. Recurrence rate was similar for both techniques. As for other complications such as wound infections, it was higher for open herniotomy compared with laproscopic herniotomy, especially in infants [8].
Though this study is not a comparative study, we have analyzed the outcome of an open one-stitch technique in comparison to other studies.
The male/female ratio in our study was 8.8:1. A male/ female ratio of 3:1 to 10:1 has been reported by various series [2]. In our study, 64% infants had unilateral rightsided hernia. Inguinal hernias are more common on the right side and up to 60% can be right sided [9]. The mean operative time in our series was 14.99 min, which is much shorter than that reported in other studies of laparoscopic repair of inguinal hernias. Koivusalo et al. [10] reported a mean operative time of 33 min and with unilateral laparoscopic hernia repair. Chan et al. [11] reported a mean operative time of 23 min, Schier [12] reported 22 min and Tam et al. [13] reported 23.8 min. This may be based on the fact that laparoscopic hernia repair will need creation of multiple ports and pneumoperitoneum and closure of port incisions. The operative time was shorter as compared to the open technique by Chan et al. [11] (14.99 vs. 18 min). The mean time in the OR was 38.23 min, which was less than that reported in the study of Brown et al. [14] (i.e., 48.6–50.4 min after pediatric hernia repair). For laparoscopic hernia repair, the mean OR stay time is much higher (63 min) than that reported by Koivusalo et al. [10] This may be because laparoscopy requires a general anesthesia along with endotracheal intubation and the need for adequate paralysis. However in our series, general anesthesia was given to patients using laryngeal mask airway and caudal analgesia was given for pain. Patients were not paralyzed. As such the stay in the OR relatively shortened.
The need for rescue analgesia reflects pain after inguinal surgery in children. During first 6 h of the procedure, 8% patients required a single dose of analgesia. In our study, 10% patients required a single analgesic dose over the 24 h period and 6% required two or more doses over the 24 h period. This is significantly less as compared to that reported in the study by Koivusalo et al. [10] (postoperative analgesia requirement in 79% patients). It was seen that 34% patients required two or more doses of fentanyl after laparoscopic hernia repair. This may be because in all our patients caudal analgesia was used, hence reducing the need for postoperative analgesia. Moreover, the surgical technique itself is minimally invasive involving a very small skin incision with minimal tissue handling.
The overall mean cosmesis score was 2.98, which was rated as excellent during 6 months, 1 year and 2 years follow-up. In the study by Koivusalo et al. [10], (eightynine patients were enrolled (laparoscopic hernia repair: 47, open repair: 42), the scores of scar cosmesis 2 years after surgery were found to be in favor of open repair The median times in the operation room for laparoscopic hernia repair and open repair were 63 and 38 min, respectively. Other characteristics including age were similar to our study. This is in contrast to those reported by studies of Chan et al. [11] and Schier [12], where use of smaller instruments in the laparoscopic group was responsible for better cosmetic appeal in laparoscopic hernia repair group. In our study, the cosmesis was excellent because of a small incision, minimal tissue handling and avoidance of any skin sutures by using a single U-stitch for external oblique and Scarpa’s fascia closure and skin edge approximation.
None of our patients had a recurrent hernia on followup. However, one patient developed a scrotal hydrocele 30 months after herniotomy. A groin ultrasound ruled out recurrence. The overall recurrence after an uncomplicated hernia repair has been estimated to be between 0% and 0.8%. A higher incidence of recurrent hernias ranging from 0.41% to 4% has been reported after laparoscopic hernia repair [9,11,13,14]. Eleven percent of patients developed a contra lateral hernia on follow-up. These included 7 males (8%) and 3 females (33%). Tsai et al. [15] reported a 10% incidence of contralateral metachronous inguinal hernia after open hernia repair over a 2 year follow-up period. Ron et al. [16] estimated a 7.2% risk of developing a metachronous contralateral inguinal hernia.
Although the advantage of laparoscopy lies in the fact that it can identify the Contralateral Patent Processus Vaginalis (CPPV). Yerkes et al. [17] in a series of 627 patients on laparoscopy found that the CPPV was present in 46% patients <1 years of age and in 39% patients >1 year of age. Geisler et al. [18] estimated the incidence of CPPV to be 33%. The incidence of a CPPV was found to be more in females as compared to males (44.7% vs. 22%) [11]. However, the number of patients among these who developed clinical inguinal hernias is not exactly known.
As we can infer from the comparison with the above studies, the operating time, stay in OR, and analgesic requirement were less with our technique when compared to laparoscopic hernia repair. This reduces the total procedure costs. Moreover, the material costs in terms of instruments, wound closure (closure of multiple port sites in laparoscopy compared to a one-stitch closure in our technique) and dressings are also higher in laparoscopic hernia repair as compared to our technique. The technique thus proves to be quite useful in developing countries in centers where laparoscopy is not a routine, providing excellent cosmesis and low-cost inputs.
Conclusion
Laparoscopic herniotomy for management of indirect inguinal hernia in children needs expertise and equipment and is associated with a long learning curve. One-stitch herniotomy can be considered a suitable alternative that is resource friendly and cost-effective. There is no need for costly equipment and it can be performed as a day care procedure. Outcome as shown in our series in terms of cosmesis is excellent at 2 years follow-up with minimal risks and complications.
References
- Rowe MI, Copelson LW, Clatworthy HW. The patent processus vaginalis and the inguinal hernia. J Pediatr Surg 1969; 4: 102-107.
- Wiener ES, Touloukian RJ, Rodgers BM, et al. Hernia survey of the section on surgery of the American Academy of Pediatrics. J Pediatr Surg 1996; 31: 1166-1169.
- Ladd WE, Gross RE. Abdominal Surgery of surgery of infancy and childhood. Philadelphia: WB Saunders; 1941.
- Levitt MA, Ferraraccio D, Arbesman MC, et al. Variability of inguinal hernia surgical technique: A survey of North American pediatric surgeons. J Pediatr Surg 2002; 37: 745-751.
- Bharathi RS, Arora M, Baskaran V. Pediatric inguinal hernia: Laparoscopic versus open surgery. JSLS 2007:12: 277-281.
- Udwadia TE. Hence this special issue. Ind J Surg 2003; 65: 20-21.
- Bose SM. Changing face of health care and our responsibilities. Ind J Surg 2003; 65: 17-19.
- Esposito C, Peter SD, Escolino M, et al. Laparoscopic versus open inguinal hernia repair in pediatric patients: A systematic review. J Laparoendosc Adv Surg Tech A 2014; 24: 811-818.
- Rowe MI, Clatworthy HW. Incarcerated and strangulated hernias in children. A statistical study of high risk factors. Arch Sur 1970; 101: 136-139.
- Koivusalo AI, Korpela R, Wirtavuori K, et al. A single-blinded, randomized comparison of laparoscopic versus open hernia repair in children. Pediatrics 2009; 123: 332-337.
- Chan KL, Hui WC, Tam PK. Prospective randomized single-center, single-blind comparison of laparoscopic vs. open repair of pediatric inguinal hernia. Surg Endosc 2005; 19: 927-932.
- Schier F. Laparoscopic inguinal hernia repair-a prospective personal series of 542 children. J Pediatr Surg 2006; 41: 1081-1084.
- Schier F, Montupet P, Esposito C. Laparoscopic inguinal herniorrhaphy in children: a three-center experience with 933 repairs. J Pediatr Surg 2002; 37: 395-397.
- Chan KL, Chan HY, Tam PK. Towards a near-zero recurrence rate in laparoscopic inguinal hernia repair for pediatric patients of all ages. J Pediatr Surg 2007; 42: 1993-1997.
- Tsai YC, Wu CC, Yang SS. Open versus minilaparoscopic herniorrhaphy for children: a prospective comparative trial with midterm follow-up evaluation. Surg Endosc 2010; 24: 21-24.
- Ron O, Eaton S, Pierro A. Systematic review of the risk of developing a metachronous contralateral inguinal hernia in children. Br J Surg 2007; 94: 804-811.
- Yerkes EB, Brock JW, Holcomb GW, Morgan WM. Laparoscopic evaluation for a contralateral patent processus vaginalis: Part III. Urology 1998; 51: 480-483.
- Geisler DP, Jegathesan S, Parmley MC, et al. Laparoscopic exploration for the clinically undetected hernia in infancy and childhood. Am J Surg 2001; 182: 693-696.