Current Pediatric Research
International Journal of Pediatrics
Age-specific foreskin development before adolescence in boys.
Seong Hyeon Yu, Ho Song Yu, Sun-Ouck Kim*
Department of Urology, Chonnam National University Medical School, Gwangju, Republic of Korea.
- Corresponding Author:
- Sun-Ouck Kim
Department of Urology
Chonnam National University Medical School, 8, Hak-dong
Dong-gu, Gwangju 501-757, Republic of Korea
Tel: +82-62-220-6705
Fax: +82-62-227-1643
E-mail: seinsena@hanmail.net
Accepted date: January 30, 2017
Purpose: We examined the external genitalia of boys to estimate the age-specific prevalence of foreskin development before adolescence. Materials and methods: A total of 189 boys aged 0 to 13 years were enrolled in this study. The boys were categorized into four groups according to their age (group 1-4). The foreskin condition was classified as type I (normal prepuce), type II (adhesion of prepuce), type III (partial phimosis) and type IV (phimosis). Other abnormalities of the genitalia were also recorded. All the examinations were performed by the same urologist. Results: The incidence of type I foreskin was 46.6% in group 1 (age 0-1 year), 50.6% in group 2 (2-5 years), 77.3% in group 3 (6-9 years) and 46.2% in group 4 (10-13 years). The incidence of type IV foreskin was 20.7% in group 1, 19.3% in group 2, 4.5% in group 3 and 53.8% in group 4. Of the genital abnormalities, cryptorchidism was the most common (n=96), followed by hydrocele (n=61). Conclusion: Physiologic phimosis showed a tendency to decrease with age up to 10 years. Most of the boys with phimosis did not require treatment.
Keywords
Development, Foreskin, Phimosis, Prepuce.
Introduction
The foreskin, the anatomical covering of the glans, is composed of an outer keratinized layer and an inner mucosal layer, lining a preputial sac [1,2]. The foreskin is thought to primarily protect the glans and urethral meatus, thus decreasing external irritation or contamination [3].
Phimosis is recognized as the inability to retract the prepuce because of preputial adhesion to the glans penis. It is common in the newborn and infants, but this state is transient and resolves in nearly all boys [1,3]. Moreover, several studies reported that the degree of preputial retractability increases with age and varies considerably among individuals [1,3,4].
Many parents are concerned about phimosis in their children and consider this condition as an indication for circumcision. However, there is considerable debate among doctors with regard to the indication for circumcision [5]. Moreover, many authors suggest that routine circumcision is not necessary [6,7]. Nevertheless, no studies have been published recently about foreskin development in Korean boys. Therefore, we examined the age-specific prevalence of foreskin development before adolescence.
Material and Methods
Study Population
We prospectively reviewed 189 boys aged 0 to 13 years between March 2013 and December 2015 who visited pediatric urology clinics due to get urologic examinations in Chonnam National University Hospital. The boys were categorized into four groups according to their age: group 1 (0 to 1 years, infants; n=58), group 2 (2 to 5 years, preschool boys; n=83), group 3 (6 to 9 years, low grade elementary school boys; n=22) and group 4 (10 to 13 years, high grade elementary school boys; n=26).
All boys underwent physical examination, which included the evaluation of external genitalia for abnormalities. Before the manual retraction of the prepuce, the status of the preputial covering over the glans was evaluated. Subsequently, the prepuce of each subject was examined using gentle retraction without traumatic force and the degree of preputial retractability and other abnormalities of the external genitalia were recorded. All the examinations were performed by the same urologic specialist. All participants or the parents of the child provided written informed consent with data collection, and the study received approval from the local ethics committee and the institutional review board. The study procedures complied with the guidelines provided by the Declaration of Helsinki.
Classification of the Foreskin
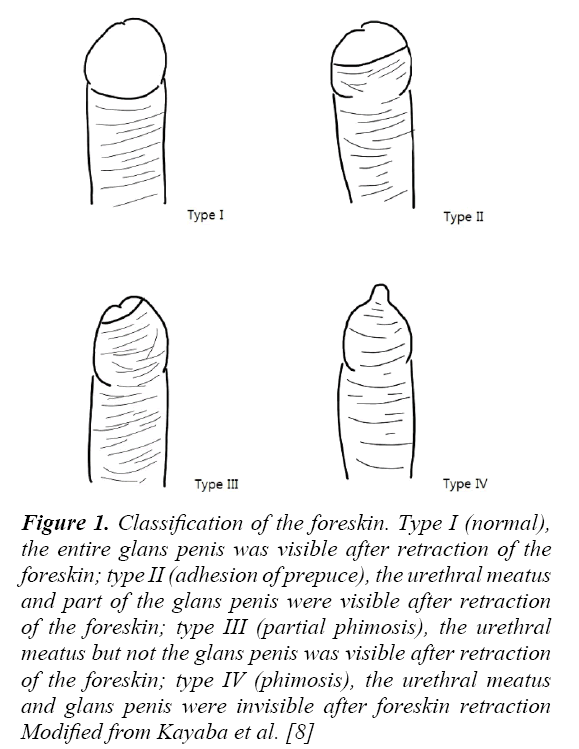
The classification of the foreskin used in this study was proposed by Hsieh et al., which was modified from Kayaba et al.’s study [8]. The foreskin`s condition was classified as type I (normal, the entire glans penis was visible after retraction of the foreskin), type II (adhesion of prepuce, the urethral meatus and part of the glans penis were visible after retraction of the foreskin), type III (partial phimosis, the urethral meatus but not the glans penis was visible after retraction of the foreskin), and type IV (phimosis, the urethral meatus and glans penis were invisible after retraction of the foreskin) [1,8]. The foreskin types are illustrated in Figure 1.
Figure 1: Classification of the foreskin. Type I (normal), the entire glans penis was visible after retraction of the foreskin; type II (adhesion of prepuce), the urethral meatus and part of the glans penis were visible after retraction of the foreskin; type III (partial phimosis), the urethral meatus but not the glans penis was visible after retraction of the foreskin; type IV (phimosis), the urethral meatus and glans penis were invisible after foreskin retraction Modified from Kayaba et al. [8]
| Age Group | Prepuce Type n (%) |
Total (n=189) |
|||
|---|---|---|---|---|---|
| Type I | Type II | Type III | Type IV | ||
| 1 (0-1 year) | 27 (46.6%) | 9 (15.5%) | 10 (17.2%) | 12 (20.7%) | 58 |
| 2 (2-5 years) | 42 (50.6%) | 12 (14.5%) | 13 (15.7%) | 16 (19.3%) | 83 |
| 3 (6-9 years) | 17 (77.3%) | 3 (13.6%) | 1 (4.5%) | 1 (4.5%) | 22 |
| 4 (10-13 years) | 12 (46.2%) | 0 | 0 | 14 (53.8%) | 26 |
| p-value <0.001 (by χ2-test) | |||||
Table 1: Foreskin presentation in the boys
Statistics
Statistical analyses were performed using SPSS ver. 17.0 (SPSS, Chicago, IL, USA). The χ2-test was used to analyze the foreskin distribution in the four groups. Statistical significance was set at p<0.05 for all analyses.
Results
Age-Specific Prevalence of Foreskin Development
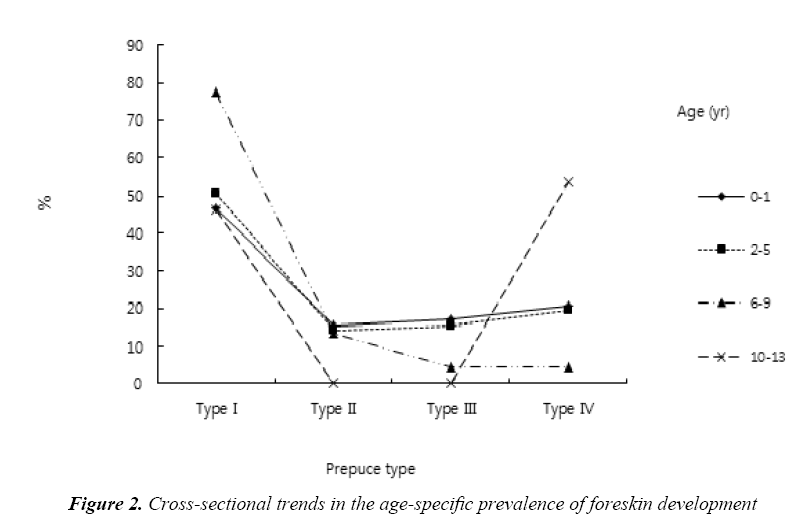
None of the boys had undergone circumcision. The incidence of type I foreskin was 46.6% in group 1 (aged 0 to 1 year), 50.6% in group 2 (2 to 5 years), 77.3% in group 3 (6 to 9 years), and 46.2 % in group 4 (10 to 13 years). The incidence of type IV foreskin was 20.7% in group 1, 19.3% in group 2, 4.5% in group 3, and 53.8% in group 4 (Table 1). With regard to cross-sectional trends in the age-specific prevalence of foreskin development, the prevalence of type I foreskin increased with age from 46.6% in group 1 to 50.6% in group 2 and 77.3% in group 3. In contrast, the prevalence of type IV foreskin decreased with age from 20.7% in group 1 to 19.3% in group 2 and 4.5% in group 3. Type II and III showed no particular trends with age (Figure 2). The p-value for the distribution of foreskin development by age groups was <0.001.
| Age Group (n) | Total (n=189) |
||||
|---|---|---|---|---|---|
| 1 (0-1 year) | 2 (2-5 years) | 3 (6-9 years) | 4 (10-13 years) | ||
| Hydrocele | 8 | 39 | 11 | 3 | 61 |
| Cryptorchidism | 44 | 39 | 9 | 4 | 96 |
| Hypospadias | 3 3 |
4 1 |
0 2 |
3 16 |
10 22 |
| Others | |||||
Table 2: Abnormalities found among the boys
Abnormalities in the Boys
Visible abnormalities among the 189 boys included hydrocele, cryptorchidism, hypospadias and others; and cryptorchidism was the most common (n=96). Other diagnoses included varicocele, inguinal hernia, and balanoposthitis.
This study found that physiologic phimosis showed a tendency to decrease with age up to 10 years and very few boys had an unretractable prepuce by the age of 13 years. This result provides further information about foreskin development before adolescence and may help urologists to better treat and explain the foreskin`s condition in daily practice. In addition, with the understanding of normal preputial development, unnecessary circumcision and anesthesia may be prevented in boys before adolescence.
Preputial separation from the glans is a developmental process and begins by 24 weeks of gestation. The degree of preputial retractability varies considerably among individuals [4]. However, in general, young children have a higher prevalence of preputial covering. This might be explained by the fact that the immature glans of young children is more vulnerable and needs more protection from chemical or mechanical injuries [3].
To date, few studies focusing on foreskin development in school-aged boys have been published [1,3,8]. Our study provides further information that could be used to clinically explain foreskin development. Our results indicate that the degree of preputial retractability increases with age, while the prevalence of unretractable prepuce decreases with age. These findings correspond with the study by Kayaba et al. who reported on foreskin development in 603 Japanese boys and found that the prevalence of unretractable foreskin (type III and IV) decreased from 70% at the age of 6 months to less than 10% after 5 years of age [8]. Another study conducted in Taiwan by Hsieh et al. reported on foreskin development in 2149 elementary school boys and found that 49.9% of the boys at age 7 years, 34.8% at age 10 years, and 8.0% at age 13 years, had unretractable foreskin [1]. In addition, Ko et al. [3] examined foreskin development in 1145 Taiwanese boys and reported that the prevalence of unretractable foreskin decreased with age, with rates of 83.1%, 4.5%, 1.5%, and 0.3% in subjects aged 0, 7, 10, and 13 years, respectively. The decrease in the prevalence of unretractable foreskin with increasing age suggested that the rate of physiological phimosis and the frequency of spontaneously resolved phimosis are very high among boys. Therefore, this should be considered when treating school-aged boys with phimosis. In addition, this prevalence are different for each subjective study. Such a discrepancy could be due to several reasons. First, the physical examination was performed by different physicians. Second, the force used to retract the prepuce and the interpretation of preputial retractability may have been different among physicians.
In the present study, the physical examination was performed by a single urologic specialist using the same classification.
The increase in the frequency and duration of physiologic erection in adolescence may facilitate preputial separation. Ko et al. reported that preputial development progressed more rapidly from age 10 to 13 years [3]. In an animal model of male rats, the preputial separation was revealed to be androgen-dependent and to occur around the time of puberty in male rats [9]. Horita et al. [10] reported that the frequency of nocturnal penile tumescence showed a tendency to increase with age and had a maximum frequency at 13 or 14 years of age. Moreover, tumescence time and maximum increase in penile circumference were both greater in children over 12 years compared to children below 10 years of age [10]. However, in the present study, boys aged 10 to 13 years were less likely to have a type I prepuce than boys aged 6 to 9 years. This result might be due to differences in the investigation group.
Circumcision is one of the most commonly performed procedures in males. An indication for circumcision in the young boy includes the pathologic phimosis, balanophosthitis or recurrent urinary tract infections thought to be associated with the redundant preputial skin. The American Academy of Pediatrics reported that although neonatal circumcision had potential medical benefits and advantages, it also had disadvantages and risk [6]. The medical advantages of circumcision include the prevention of urinary tract infection, balanoposthitis, pathologic phimosis and penile cancers. However, the medical disadvantages of circumcision include pain, the necessity of anesthesia, and potential contraindications and complications [3]. Indeed, the prevalence of circumcision differs from country to country. In the United States, approximately 58.3% of newborns were circumcised in 2010 [11]. In Canada, circumcision rates are relatively low, ranging from 10% to 30% [12]. In Taiwan, the prevalence of circumcision among school boys was 7.67% on average, and the cumulative national circumcision rate in Denmark was approximately 1.6% by the age of 15 years [3,13]. In Korea, no studies reporting the prevalence of circumcision in schoolboys have been published. Studies on the prevalence of circumcision in Korean boys are needed.
Many parents are concerned about the unretractable prepuce of their children and have their children circumcised for this reason. With regard to the indications for circumcision, the proportions of procedures indicated for phimosis ranged from 80.6% to 90.2%. However, Rickwood et al. highlighted the difference between physiologic phimosis, an unscarred pliant preputial narrowing or normal adhesion of the prepuce to glans and pathologic phimosis, a condition characterized by secondary cicatrization of the orifice [3,14]. Therefore, they reported that the only absolute indication for circumcision is rarely experienced before the age of 5 years, affecting approximately 0.6% of boys [15].
The boys in the present study had various urologic diseases. Among these, cryptorchidism was the most common, followed by hydrocele. Other diagnoses included hypospadias, varicocele, inguinal hernia and balanoposthitis. To date, no studies focusing on the relationship between pediatric urologic disease and foreskin development have been published. Therefore, further studies on this relationship are needed.
Our study had a number of limitations. First, the number of boys for this study was not sufficiently large. The observation in this study took place in a hospital and not in a school. Increasing the number of boys might provide stronger evidence for our conclusion. Second, we examined the foreskin using gentle retraction without attempting to identify the tightness of the prepuce in this study because this was too cumbersome to perform by only one physician without the aid of the boys’ parents.
Conclusion
Physiologic phimosis showed a tendency to decrease with age up to 10 years and only few boys had an unretractable prepuce by the age of 13 years. Most of the boys with phimosis did not require any treatment.
References
- Hsieh TF, Chang CH, Chang SS. Foreskin development before adolescence in 2149 schoolboys. Int J Urol 2006; 13: 968-970.
- Cold CJ, Taylor JR. The prepuce. BJU Int 1999; 83: 34-44.
- Ko MC, Liu CK, Lee WK, et al. Age-specific prevalence rates of phimosis and circumcision in Taiwanese boys. J Formos Med Assoc 2007; 106: 302-307.
- Gairdner D. The fate of the foreskin, a study of circumcision. Br Med J 1949; 2: 1433-1437.
- Farshi Z, Atkinson KR, Squire R. A study of clinical opinion and practice regarding circumcision. Arch Dis Child 2000; 83: 393-396.
- Anonymous. American Academy of Pediatrics: Report of the task force on circumcision. Pediatrics 1989; 84: 388-391.
- Poland RL. The question of routine neonatal circumcision. N Engl J Med 1990; 322: 1312-1315.
- Kayaba H, Tamura H, Kitajima S, et al. Analysis of shape and retractability of the prepuce in 603 Japanese boys. J Urol 1996; 156: 1813-1815.
- Korenbrot CC, Huhtaniemi IT, Weiner RI. Preputial separation as an external sign of pubertal development in the male rat. Biol Reprod 1977; 17: 298-303.
- Horita H, Kumamoto Y, Aoki M, et al. Clinical significance and usefulness of measuring nocturnal penile tumescence in children. Nihon Hinyokika Gakkai Zasshi 1991; 82: 1939-1946.
- http://www.childtrends.org/?indicators=infant-male-circumcision
- Quayle SS, Coplen DE, Austin PF. The effect of health care coverage on circumcision rates among newborns. J Urol 2003; 170: 1533-1536.
- Frisch M, Friis S, Kjaer SK, et al. Falling incidence of penis cancer in an uncircumcised population (Denmark 1943-90). BMJ 1995; 311: 1471.
- Rickwood AM, Kenny SE, Donnell SC. Towards evidence based circumcision of English boys: Survey of trends in practice. BMJ 2000; 321: 792-793.
- Shankar KR, Rickwood AM. The incidence of phimosis in boys. BJU Int 1999; 84: 101-102.